SAN FRANCISCO - CT perfusion (CTP) imaging has a pretty good track record for estimating salvageable brain tissue after a stroke by measuring cerebral blood-flow patterns. But the newest research frontier is more ambitious, creating a brain atlas to predict which patients will recover, which ones won't, and which abilities patients might expect to regain, according to a Wednesday presentation at the International Symposium for Computed Tomography (ISCT).
At Massachusetts General Hospital (MGH), the nascent atlas project has scored some early victories in the battle to restore patients' lives following acute stroke.
Targeting tPA therapy
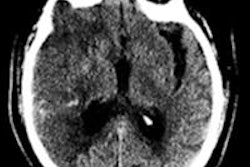
The cerebral blood flow (CBF) parameters for predicting acute stroke outcomes after thrombolytic therapy with tissue plasminogen activator (tPA), based on quantitative CT perfusion imaging, as published in 2006 by Schaefer, Lev, and colleagues, have turned out to be good outcomes predictors in practice, said Dr. Michael Lev, MGH's director of emergency neuroradiology.
Schaefer, Lev, and colleagues found that quantitative CTP could distinguish ischemic tissue likely to infarct from tissue likely to survive (American Journal of Neuroradiology, January 2006, Vol. 27:1, pp. 20-25).
Typically, core with greater than 80% reduction in cerebral blood flow will infarct, while penumbra with less than 50% CBF will never infarct, and "anything in between those two extremes is penumbra that may infarct -- it's potentially salvageable tissue and that's our target for therapy," Lev said.
With speed, skill, well-targeted treatment, and a little luck, the core infarct area is prevented from growing significantly larger and a minimum of brain tissue is lost.
These parameters are also well-correlated to diffusion-weighted MRI (DWI-MRI), Lev said, and in recent years the facility has become more skilled in getting stroke patients from the front door to the CT scanner in much less than 30 minutes. CT perfusion doses are extremely low as well, owing to the use of iterative reconstruction, he said.
Unlike MRI, with CT, a focused clinical history is critical for making an accurate diagnosis. CTP maps cannot be interpreted in a vacuum, Lev said.
"You can have the same low density on an unenhanced head CT, and if it's acute onset hemiparesis, if it's a subtle onset of sensory symptoms in a 25-year-old woman, it might be [multiple sclerosis]," he said.
For now, CT lacks the kind of tissue-specific sensitivity that MR wields, although tissue characterization with dual-energy CT definitely has that potential, he said.
"In the future I'd like to see us getting some help in interpreting these maps," Lev said. That means a multivariate-based interpretation model.
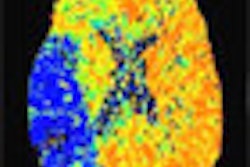
There are far more subtle measurable differences. Baseline blood flow in gray matter is twice baseline flow in white matter. There seem to be specific areas of the brain that are more vulnerable ischemically than others. MGH's atlas-based logistic modeling project aims to model outcomes in specific brain regions.
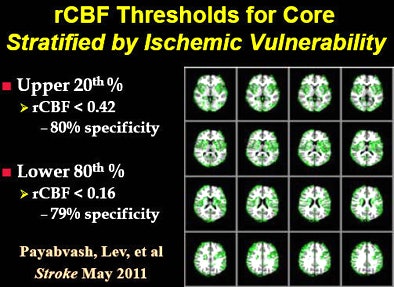 A new study maps the areas of greater ischemic vulnerability, shown in green. All images courtesy of Dr. Michael Lev.
A new study maps the areas of greater ischemic vulnerability, shown in green. All images courtesy of Dr. Michael Lev.
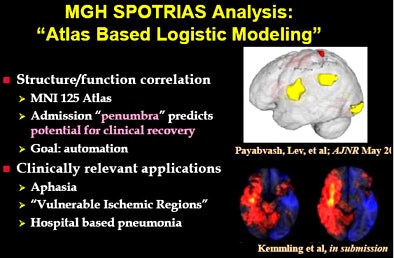 MGH's atlas-based logistic modeling project aims to model outcomes probabilities in specific brain regions in stroke patients.
MGH's atlas-based logistic modeling project aims to model outcomes probabilities in specific brain regions in stroke patients.These are clues that understanding regional differences in blood flow in the brain could be helpful in predicting patient outcomes, Lev said. And it's clear that there's a lot more variability in brain regions than can be predicted by a single 50% or 80% cerebral blood-flow threshold.
"We'd like to make best-case/worst-case maps, and that's exactly what we're doing" with a grant in the U.S. National Institutes of Health's Specialized Programs of Translational Research in Acute Stroke (SPOTRIAS) program, Lev said. "We don't just want to know the probability of tissue death on a voxel-by-voxel basis, we want to know how that actually translates into clinical outcomes. So we've been building models using similar techniques to MR voxel-based or regional-based morphology, where we coregister whole-brain CTP datasets to standard atlases and parcel the brain into functional areas that correlate with outcomes," Lev said.
Beyond predicting regions of tissue death in the event of successful reperfusion of vessels, "can we predict aphasia recovery, or motor recovery, just from the admission CT perfusion dataset?" he said.
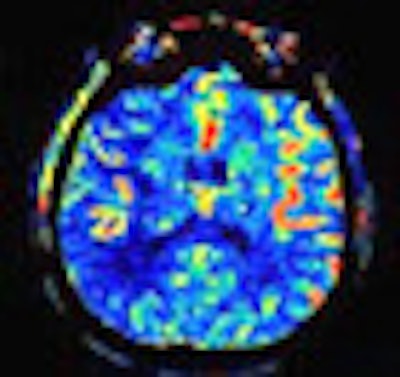
One recent MGH study looked at the pneumonia center in the brain, dividing the 430 patients into two matched groups: one that developed hospital-acquired pneumonia (HAP) following acute stroke, and another group that did not. The voxel-based analysis aimed to determine which brain regions correlated with pneumonia.
The culprit region turned out to be the right insula, which was interesting, Lev said, because the same brain region was previously implicated in sudden cardiac death following stroke. The earlier heart study, based on MRI datasets, found that the autonomic regulation of heart rate seemed to be centered in the vagus nerve centers in the right insula.
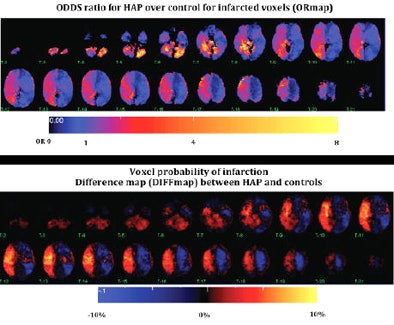 A recent MGH study found a significant correlation between right insula infarct and the development of hospital-acquired pneumonia.
A recent MGH study found a significant correlation between right insula infarct and the development of hospital-acquired pneumonia."We've actually found a similar region in the right insula that seems to be correlated with aspiration pneumonia," though the incidence of HAP may be related to dysphagia or other confounding factors, he said. "There has also been some speculation that T-cell and immune modulation may actually be controlled by the right insula as well," Lev said.
Though these associations remain unproven, they raise intriguing possibilities.
Another recent study used location-weighted atlas-based analysis of the association between areas of infarct and language skills recovery after stroke (Payabvash, Lev, et al, American Journal of Neuroradiology, October 2010, Vol. 31:9, pp. 1661-1668).
"We were able to show not just in the insula, but other correlative areas of the brain where perfusion thresholds below a certain amount in specific regions were able to predict likely or unlikely recovery from aphasia," Lev said. "This is all not ready for prime time, but it's stuff that we're leading up to in the future."
Models created so far include aspiration pneumonia, aphasia, and motor recovery, he said. The brain region they all have in common is the insula.
"The insula seems to be almost a canary in the coal mine for bad versus good outcomes," he said.
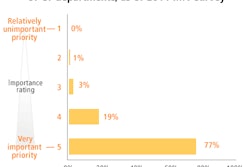
The group used stepwise binary logistic regression in 161 patients to evaluate which variables are independent predictors of clinical improvement in occlusive stroke. Age, the laterality or side of the infarct, admission NIHSS (National Institutes of Health Stroke Scale) score at admission, and the extent to which the insula index is affected were all significant predictors.
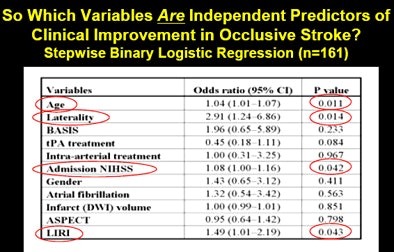 Binary logistic regression analysis of 161 patients looked for independent predictors of stroke recovery.
Binary logistic regression analysis of 161 patients looked for independent predictors of stroke recovery."With just a couple of variables, we really have been able to separate out patients who are too good to treat, because they are highly likely to get well, versus patients who are too bad to treat, whose imaging and clinical presentation means they are probably going to do poorly no matter what," Lev said. "And all the people in the middle are the ones to whom we target the therapy."