WASHINGTON, DC - To treat or not to treat? Boston researchers are increasingly confident that they can predict treatment outcomes in patients with ischemic stroke of the middle cerebral artery by measuring infarct size in the insula at CT, according to a presentation at the International Symposium on Multidetector-Row CT.
This simple conclusion, in the works for years and still awaiting final validation in randomized trials, could be a gold mine in terms of directing better stroke decision-making, according to Dr. Michael Lev from Massachusetts General Hospital (MGH).
"This is a work in progress with regard to using the CT applications, but it's really the culmination of things I've been doing for many years," said Lev, who is director of the Emergency Neuroradiology and Radiology Neurovascular Lab at MGH and an associate professor of radiology at Harvard Medical School.
No automatic decision
The decision to attempt reperfusion in ischemic stroke patients is never automatic, owing to the risk of hemorrhage if anticoagulants are given to the wrong patient -- or simply an unlucky patient, for that matter. But choosing the right patient for reperfusion therapy can minimize the risk.
Some stroke outcome predictors are well-established. For example, when a head CT or perfusion CT scan shows more than one-third of a hemisphere or more than about 70 mL to 100 mL of total infarct volume, outcomes have been poor in "study after study after study," Lev said.
Simply put, it means that physicians shouldn't recanalize if the infarct volume is too large. Conversely, studies show that patients with smaller infarct volumes have mixed rather than routinely poor outcomes, he said.
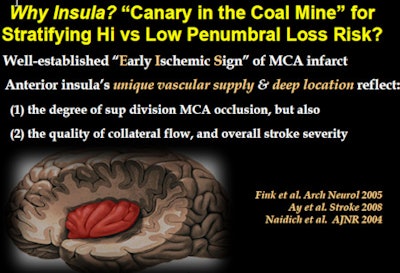
As for perfusion mismatch, its presence identifies brain tissue at risk, but it really doesn't stratify low or high risk. This new idea is different, Lev said. It refines the treatment risk-assessment process by focusing on a single central and highly vascularized brain region: the insula.
"A very simple imaging sign that we're all familiar with can actually be used to make very powerful predictions about not only stroke outcome, but who's going to respond to intra-arterial therapy and who isn't," he said. "What it comes down to is using the insula as a biomarker to potentially show patients who could benefit from reperfusion."
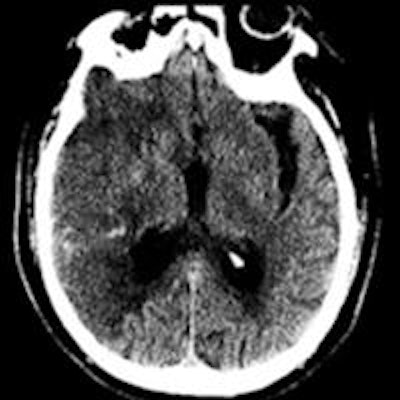
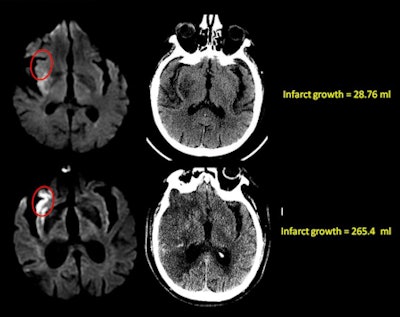 Diffusion-weighted MRI (left) and follow-up MDCT (right) of two stroke patients with similar infarct volumes; the only major difference was in involvement of the insula. The patient shown in the top row of images had no insular involvement; the patient shown in bottom row had full involvement of the anterior insula. Two-day follow-up with CT (right images) showed that infarct volume had grown by only 28.76 mL in the patient without insular involvement (top right), but infarct growth reached 265.4 mL in the patient with involvement of the anterior insula (bottom right). All images courtesy of Dr. Michael Lev.
Diffusion-weighted MRI (left) and follow-up MDCT (right) of two stroke patients with similar infarct volumes; the only major difference was in involvement of the insula. The patient shown in the top row of images had no insular involvement; the patient shown in bottom row had full involvement of the anterior insula. Two-day follow-up with CT (right images) showed that infarct volume had grown by only 28.76 mL in the patient without insular involvement (top right), but infarct growth reached 265.4 mL in the patient with involvement of the anterior insula (bottom right). All images courtesy of Dr. Michael Lev.The discovery came from a search for biomarkers in CT perfusion images that could predict stroke outcomes. "As we went through model after model, one of the surprises was that the insula came out as a significant predictor of stroke outcome no matter which model we built," he said.
If you're looking for improvement in aphasia, it's not surprising that the insula, which controls language function, is involved. The insula also plays a key role in predicting motor improvement poststroke, along with other better-known regions.
In fact, a study of two groups of 215 stroke patients who were almost identical except for insular involvement fared very differently in terms of hospital-acquired pneumonia. Patients who got it almost all had involvement of the right insula in ischemic stroke. "And that's not surprising because the right insula controls swallowing function, autonomic function," Lev said.
The starkly different pneumonia outcomes pointed not to swallowing ability as the cause, but to a possible role for right insular involvement in impaired T-cell modulation, yet another case where the insula may be a key player, he said. Earlier work showed that the right insula can also control arrhythmias and vagus nerve function.
A perfusion analysis also identified the insula as the highest ranking among cortical gray-matter regions for vulnerability to ischemia, Lev said.
"So we know from the very first stroke papers in CT ... that the insula is one of the first things you see infarct in middle cerebral artery infarction," Lev said. "We postulated that the insula was really the canary in the coal mine -- that it infarcts before other regions of the brain at risk in the setting of middle cerebral artery stroke."
Dr. Seyedmehdi Payabvash, Lev, and colleagues showed that patients with very similar strokes except for the presence of insular involvement were demonstrating very different outcomes. Patients with insular involvement had significantly greater infarct growth into the penumbra in the subsequent 24 hours.
In one example shown to attendees, a 51-year-old patient with a T-lesion had 100% of the anterior insula infarcted at admission CT; the rest of the infarct was small. There was significant infarct growth of 60%. A younger man had a very similar T-lesion and similar involvement of the basal ganglia but no insular involvement. His lesion grew only 13% in 48 hours, Lev said.
"It turned out the 25% [insular involvement] threshold was the threshold for infarct tissue growth versus no tissue growth," he said, adding that the results were both well-dichotomized and definitive. Patients who had zero to 25% insular infarct at admission had very little infarct growth, while patients with 25% to 100% insular involvement ended up with very large infarcts in the subsequent two days.
Finally, Lev and colleagues validated the results in a different consecutive intra-arterial thrombolysis cohort of 66 patients, all of whom had previously been examined with diffusion-weighted MRI (DWI-MRI) and found to have infarcts smaller than 70 mL.
The retrospective analysis showed that differences in outcomes were maintained in this cohort, both in terms of infarct growth and clinical worsening, based on whether there was more or less than 50% involvement of the anterior insula at admission. Intraobserver variability for these outcomes was also impressive (k = 0.94), Lev said.
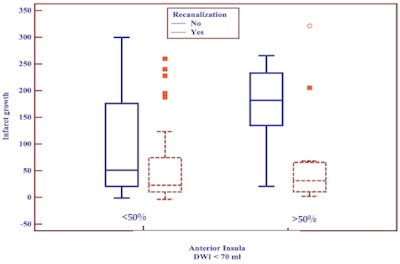 Above, in a cohort of 66 stroke patients imaged with CT, infarct growth postadmission was significantly greater in patients with more than 50% anterior insular involvement at admission. Below, clinical worsening was greater in patients with significant insular involvement in ischemic stroke.
Above, in a cohort of 66 stroke patients imaged with CT, infarct growth postadmission was significantly greater in patients with more than 50% anterior insular involvement at admission. Below, clinical worsening was greater in patients with significant insular involvement in ischemic stroke.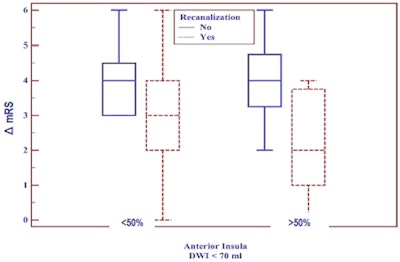
Patients with more than 50% involvement at admission had a median infarct growth of about 50 mL when recanalization was successful, compared with 200 mL when it was unsuccessful, he said. On the other hand, patients with less than 50% involvement at admission -- whether or not recanalization was successful -- had low infarct growth with a median of 50 mL.
"The bottom line here is that we looked at clinical outcome scores in addition to tissue loss and infarct growth, and the same relationship held," Lev said. "This is all a work in progress, it is all being validated with both CT and [DWI-MRI], but we think it could be a very simple, useful tool for making thrombolysis decisions in terms of gauging the risk of treatment versus the potential benefit of treatment."