In a twist that could add fuel to the debate on incidental findings, Boston researchers found that following lung nodules detected incidentally at cardiac CT produces far too little benefit for the cost incurred, according to a model analysis presented on Friday at the Society of Cardiovascular Computed Tomography (SCCT) meeting in Denver.
The Massachusetts General Hospital (MGH) study analyzed the costs, effectiveness, and cost-effectiveness of following lung nodules seen at coronary CT angiography (CTA) in the full chest field-of-view, compared with ignoring them. So how much does the average heart scan patient gain from undergoing CT follow-up of these nodules?
"The gain in life expectancy is about 10 days," said Dr. Alexander Goehler, PhD, a radiologist at MGH and senior scientist at the hospital's Institute for Technology Assessment. Worse, he said, the effort costs hundreds of thousands of dollars per life-year gained.
A handful of previous studies has addressed the issue, generally finding low direct medical costs of follow-up. But Goehler and colleagues said that those studies didn't look at the whole cost-benefit picture.
The authors believe their microsimulation model offers a more comprehensive view of the (high) costs and (limited) life-expectancy benefits associated with nodule follow-up. The model is a multiyear effort, undertaken with the National Cancer Institute (NCI), that enables the simulation of lung cancer levels in a population, Goehler explained in an interview with AuntMinnie.com.
The model predicts the remaining life expectancy, causes of death, and costs associated with follow-up and treatment of lung nodules. The data came from a cohort of 591 patients who underwent routine coronary CTA; the patients had incidental lung nodules that required follow-up but no history of malignancy.
Built on the results of the Mayo Clinic's large lung cancer study (Swenson et al, 2003), the model takes a hypothetical patient cohort "and pushes them back about 30 years to analyze the development of nodules," Goehler said. "Luckily, most don't become cancer."
The mean age of the population was 58.4 ± 10.2 years (66% male), consisting of 27% current smokers, 32% former smokers, and 22% with coronary artery disease.
Goehler and colleagues determined that following all lung nodules 4 mm and larger led to the detection of 17 malignancies among the 591 patients. Following the entire cohort using the model led to 19 deaths from lung cancer (including 232 from coronary heart disease), compared with 20 deaths from lung cancer (231 from coronary heart disease) when the incidentally detected nodules were ignored.
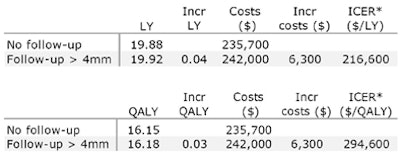
The model predicted a mean quality-adjusted life expectancy of 17.23 additional years, at a lifetime cost of $243,400, for the follow-up group, compared with 17.21 years (total lifetime cost of $238,800) for the nonfollow-up group, Goehler said.
The incremental cost-effectiveness ratio (ICER) for follow-up versus nonfollow-up was $313,100 per quality-adjusted life-year (QALY) gained.
When the analysis was restricted to current or former smokers, the model predicted the detection of 13 malignancies and an ICER of about $294,600 per QALY for following this subgroup versus ignoring the nodules.
 |
| Restricting analysis to patients with higher risk profiles for lung cancer (current smoker or former smoker with more than five pack-years), the model predicted the detection of 13 malignancies; however, the costs per additional life-year remained high. Chart courtesy of Dr. Alexander Goehler, PhD. |
Why so high?
In part, the low effectiveness of nodule follow-up results from a high number of competing mortalities: in particular, the large number of patients in a typical cardiac CT scanning population who eventually die of heart disease, Goehler said. In the model population, 231 patients died from heart disease, while just 20 died from lung cancer.
Some previous studies that failed to look at the whole cost-benefit picture made follow-up look pretty good, according to Goehler.
For example, last year Lee and colleagues investigated incidental extracardiac findings in 151 consecutive adults undergoing coronary CT. Applying Medicare reimbursement data for further follow-up testing, they estimated additional costs of $17 per patient screened and $438 per patient with follow-up. However, altered health outcomes associated with earlier detection and treatment of lung cancer were not considered, Goehler said.
Also in 2010, Kim and colleagues identified 36 (0.31%) of 11,654 patients who underwent cardiac CT prior to their diagnosis of lung cancer. Comparing different fields-of-view, the researchers demonstrated benefits of earlier detection of the wider FOV. The study concluded that detecting the incidental findings was advisable, but it did not address the effect on life expectancy.
Of course, there is much more to setting healthcare policy and follow-up criteria than merely looking at cost-effectiveness, Goehler said.
"Cost-effectiveness analysis should never be the sole decision point for deciding for or against a strategy," he said. "There are a lot of ethical reasons and a lot of clinical reasons."
One commonly held view, for example, is that exposing the patient to ionizing radiation comes with the responsibility to follow up all potentially significant findings.
Nevertheless, "from a purely economic point of view -- thinking about limited resources to maximize the overall health of the U.S. population -- there are better ways to spend your money than to intensively follow-up lung nodules," according to Goehler.
Before the study is published, the authors plan to perform a risk-stratification analysis, he said.