Researchers have developed a tool that predicts whether coronary CT angiography (CCTA) will be successful before subjecting patients to the time, expense, and risks of scanning.
The authors' "uninterpretable risk score" (URS), based on both patient and scan factors, categorizes patients who are likely to have at least one uninterpretable coronary artery segment, helping to inform patient selection and avoid radiation exposure in patients unlikely to benefit from the scans.
"In symptomatic patients, the presence of a single uninterpretable coronary segment can create uncertainty regarding an underlying severe coronary artery disease, rendering the CCTA nondiagnostic," wrote Dr. Thomas Vanhecke, from Genesys Regional Medical Center and Ascension Health in Grand Blanc, MI, and colleagues. "Such nondiagnostic CCTA tests may prompt further testing, and create not only additional expense, but also subject patients to needless radiation" (Circulation: Cardiovascular Imaging, July 20, 2011).
Knowledge gaps
The rapid development of coronary CTA has led to knowledge gaps regarding which patient factors are likely to create an uninterpretable CCTA scan, the authors wrote. The study aimed to develop and validate a simple clinical tool to predict the prescan likelihood of obtaining coronary CTA scans with major uninterpretable coronary segments.
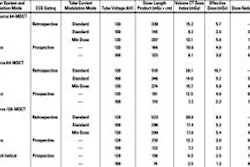
To create the URS, the researchers retrospectively looked at 8,585 symptomatic patients (mean age, 55.6 years ± 12.8; 47.8% men) referred for CCTA for evaluation of coronary artery disease. The data were used to identify the variables most strongly associated with the presence of at least one uninterpretable major coronary segment at CCTA.
The data collected to develop risk scores included information about demographics, coronary risk factors, and medical history. The information was collected by research coordinators from patient interviews and medical records. Specific questions related to a history of coronary artery disease, physical activity, and cigarette smoking history, the authors stated.
CCTA images were interpreted according to the 16-segment American Heart Association model by experienced readers, with each segment characterized as interpretable or uninterpretable, and analyzed for stenosis severity. The model was then validated among an additional 915 symptomatic patients who underwent coronary CTA at the center.
"The results of coronary artery calcium score measurement and the patient's heart rate immediately prior to CCTA acquisition are generally not available to the clinician at the point-of-decision and were not included in our primary analyses," Vanhecke and colleagues wrote. Because of its importance in scan quality, however, this information was collected and analyzed when available.
"Often CCTA studies have one or more isolated uninterpretable segments that do not render the study nondiagnostic," the group noted. "To account for this, the frequency and predictors of a 'complete nondiagnostic' CCTA result [were] analyzed as a secondary study outcome."
Among the statistical analysis steps was a weight-point system assigned to the variables based on regression coefficient values.
The URS was predictive of uninterpretable results in both the development and validation cohorts, the authors wrote. Multivariate analysis revealed seven parameters that were independent predictors of an uninterpretable coronary segment:
- Diabetes
- Hypertension
- Chronic obstructive pulmonary disease (COPD)
- Sedentary lifestyle
- Body mass index (BMI) ≥ 40 kg/m2
- Age ≥ 65
- History of atrial fibrillation
"For every four-point increase in the URS (range, 0-12), the rate of at least one uninterpretable segment per 100 CCTA studies increased ~1.5-fold," the authors wrote.
In addition, uninterpretable results were associated with three-month outcomes in the development cohort. The presence of one more uninterpretable coronary artery segment was associated with an increased frequency of subsequent hospitalization, stress testing, invasive coronary angiography, percutaneous coronary intervention, coronary artery bypass grafting, and myocardial infarction.
On the other hand, hyperlipidemia, smoking history, and male gender were eliminated from the model for lack of statistical significance. Peripheral arterial disease, congestive heart failure, and prior stroke were not included in the multivariable model because they were present in fewer than 5% of patients.
Because heart rate and coronary artery calcium scores were available in only 56% of the population, they were not included in the analysis.
The results agree with and extend the results of an earlier large study, the Rule Out Myocardial Infarction Using Computed Assisted Tomography (ROMICAT) trial, the group noted.
"In ROMICAT, the frequency of scans with one (or more) uninterpretable segment was 16.1%," they wrote. "In our study we found similar predictors of uninterpretable results including: age, diabetes, and hypertension. We extend the findings of ROMICAT by establishing BMI, sedentary lifestyle, and COPD as significant independent predictors of uninterpretable segments."
Image interpretability
Interpretability of an image depends on two sets of factors: patient-related (age, BMI, inability to control heart rate, underlying illness that increases patient motion, dyspnea, contrast allergy, etc.) and scan-related (heart rate, scanner type, experience, contrast timing, etc.), according to the authors.
"Therefore, it is unsurprising that a weighted scoring system that considers multiple factors such as the URS demonstrated predictive superiority of CCTA quality over any single factor alone," they wrote. "This is the first large-scale, multicenter study to develop and validate a risk score capable of predicting the likelihood of finding ≥ 1 uninterpretable coronary segment by CCTA."
With regard to age, even patients older than 75 years have 100% interpretable coronary artery segments, and the study does not recommend restriction of CCTA due to age alone.
The most important limitation of the study was the lack of evaluation of clinical indication or appropriateness of the test, which should not be discounted when deciding whether to scan, the group wrote. In addition, the number of patients excluded for high calcium scores was unknown and may have confounded the results, and many scanning variables were also unknown.
The results are likely to be applicable even in the face of improving technology, according to the group. "Although it is likely the future CT technology may reduce frequency of uninterpretable results, the identified factors are likely to be relational to scan quality," Vanhecke and colleagues wrote.