For as long as 2.5 years after undergoing coronary CT angiography (CCTA), invasive angiography and revascularization are uncommon, even in patients with significant coronary artery disease at CT, according to a report presented on Tuesday at the American Heart Association (AHA) meeting in Orlando, FL.
The results are a win for CCTA inasmuch as they show that the noninvasive test does not lead to overutilization of downstream invasive cardiac procedures such as angiography, coronary artery bypass grafting, and percutaneous coronary intervention.
"There's a fair amount of pure medical management in this country [without invasive measures] that I think gets often overlooked," lead investigator Leslee Shaw, PhD, told AuntMinnie.com. "One of the things that CT angiography allows is for the physician to understand the severity of disease without having to send [patients] to the cath lab."
The results represent the latest and longest-term follow-up of patients in the Coronary CT Angiography Evaluation for Clinical Outcomes (CONFIRM) registry, which examined outcomes in patients with suspected coronary artery disease (CAD). These patients typically show up in emergency departments complaining of chest pain, and in CONFIRM they received CCTA studies.
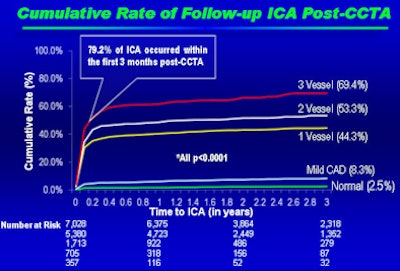
"We found very low rates of invasive angiography in normal studies, with the rates increasing for patients with one- or two-vessel disease," Shaw said. "If you had a patient with three-vessel obstructive stenosis, then the rate of invasive angiography would be about two-thirds."
If the goal of CT is to prevent invasive downstream testing and revascularization, these latest CONFIRM results "mean you have a test that's working as it should," she said. "The whole idea of a noninvasive test would be to allow selective use of invasive procedures."
Optimally, noninvasive CCTA would serve as a gatekeeper to invasive coronary angiography and limit the volume of downstream procedures. On the other hand, detection of anatomically defined CAD, even mild CAD, could lead to greater use of downstream invasive procedures. Data on the topic are sparse.
A study of Medicare claims data from nearly 300,000 older patients that appeared in the November 16 Journal of the American Medical Association, for example, found twice the rate of downstream invasive procedures in CCTA patients versus those receiving myocardial perfusion scintigraphy; however, those findings contradict previous results from the CONFIRM registry and other investigations.
Shaw's work, as well as this week's JAMA study and other research, have been undertaken because the rates of follow-up angiography and revascularization procedures following CCTA have not been well-defined.
Shaw, a professor of medicine at Emory University School of Medicine, along with Dr. James Min, from Cedars-Sinai Medical Center, and colleagues from seven other participating centers in six countries, followed 15,223 patients without known coronary artery disease for 2.4 ± 1.2 years after CCTA.
"The primary end point was to look at all-cause mortality, and the second was to look at catheterizations and revascularizations," she said.
The protocol defined severity of coronary artery disease as normal (0% luminal stenosis), mild (> 0 to < 50%), or severe (≥ 50%) stenosis in one to three vessels, or left main artery stenosis.
Rates of downstream angiography and revascularization were estimated using logistic regression models, including clinical factors for covariate adjustment. At two years post-CCTA, 2,218 angiography procedures and 1,211 revascularizations had been performed.
Over the 2.4-year follow-up period, coronary artery disease extent at baseline (left) and intervention rates post-CCTA (right) were as follows:
CAD severity at CCTA and intervention rates
|
The study found low rates of invasive angiography and interventions, even in patients with significant disease, "such that if you had three vessels with stenosis, about two-thirds of those patients went on to an invasive coronary angiogram," Shaw said.
Explaining the low patient referral rate, Shaw said the decision to intervene depends on a lot of factors that are discussed between the doctor and patient.
"Not all of them would be revascularization candidates," she said. Patients might be very ill, or they may have decided on medical management. Age and comorbidities may be a concern, or "maybe they just want to know progressive disease status," Shaw said.
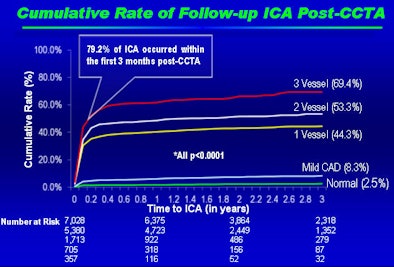 |
| Results show low rates of invasive angiography and revascularization over a mean follow-up period of 2.4 years following CCTA, with interventions rising in more severe disease. Image and data courtesy of Leslee Shaw, PhD. |
Years of experience with CCTA have shown that it allows assessment of disease severity and perhaps intensive medical management without the consequences of revascularization, she said.
Going forward, even lower revascularization rates should be possible, according to Shaw.
"We see it happen in other modalities all the time," she said. "I expect to see the [angiography referral] rates go down even lower in people with mild and moderate coronary disease as people become more confident in the results of CCTA." Even the results of this study, once published, will help clinicians understand that they can trust CCTA results and avoid unnecessary interventions, she said.
"I think you would not want to see a lot of normals or people with mild coronary disease going to the cath lab, and that's exactly what we saw," Shaw noted, adding that the recent JAMA report (Shreibati et al, November 16, 2011) on people having both CCTA and angiography strikes her as unusual.
"I think if you were going to have two procedures, you would just send the patient directly to the cath lab," she said.