A radiologic ternary classification model achieved “excellent” diagnostic performance in differentiating lung lesions on CT images, according to findings published December 23 in Radiology.
The model differentiated preinvasive lesions from minimally invasive adenocarcinoma and invasive adenocarcinoma in nonsolid nodules detected on CT images, wrote a team led by Qi Wan, MD, PhD, from the First Affiliated Hospital of Guangzhou Medical University in Guangdong, China.
“Incorporating CT attenuation and morphologic features improved model performance in predicting nonsolid nodule pathologic invasiveness compared with using diameter alone,” Wan and co-authors wrote.
Persistent nonsolid nodules present on CT images. While these nodules have slow growth patterns, they have a higher chance of malignancy compared with solid nodules. Estimating the extent of invasiveness for nonsolid nodules may affect clinical management for lung cancer patients.
Prior research suggests that radiologic features on CT, such as nodule size, attenuation, vessel changes, or presence of reticulation, could predict tumor invasiveness of nonsolid nodules. Wan and colleagues developed a radiologic ternary classification model for differentiating among lesions from nonsolid nodules.
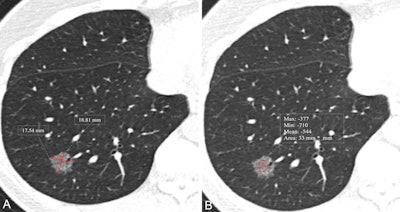 CT images show measurement of nodule size and mean CT attenuation in a 52-year-old woman. Transverse lung-window CT images were obtained without administration of contrast material. This lesion was pathologically proven to be an invasive adenocarcinoma. (A) Nodule size was measured by taking the mean of the maximum length and maximum width, defined as perpendicular to the length on the same axial image showing the maximum area of the nodule. The red lines indicate the length and width and measure 17.5 mm and 18.8 mm, respectively. (B) Nodule CT attenuation was measured by placing three regions of interest within the nodule covering two-thirds of the largest area while avoiding vessels and bronchioles. The red circle indicates CT attenuation and measures -544 HU.RSNA
CT images show measurement of nodule size and mean CT attenuation in a 52-year-old woman. Transverse lung-window CT images were obtained without administration of contrast material. This lesion was pathologically proven to be an invasive adenocarcinoma. (A) Nodule size was measured by taking the mean of the maximum length and maximum width, defined as perpendicular to the length on the same axial image showing the maximum area of the nodule. The red lines indicate the length and width and measure 17.5 mm and 18.8 mm, respectively. (B) Nodule CT attenuation was measured by placing three regions of interest within the nodule covering two-thirds of the largest area while avoiding vessels and bronchioles. The red circle indicates CT attenuation and measures -544 HU.RSNA
The final analysis included retrospective data from 1,683 patients with a median age of 53 who had 2,125 nonsolid nodules. The patients had pathologically confirmed lung adenocarcinoma and suspicious malignant nonsolid nodules measuring 3 mm to 30 mm on preoperative CT scans between 2012 and 2024.
Partial proportional odds model analysis showed that the independent radiologic factors for predicting pathologic invasiveness included average diameter, the presence of intranodular vessels, and average CT attenuation, among others.
Independent radiologic factors tied to pathologic invasiveness | |
Independent radiologic factor | Odds ratio (OR) |
Average diameter (preinvasive lesion vs. minimally invasive adenocarcinoma) | 1.3 |
Average diameter (minimally invasive adenocarcinoma vs. invasive adenocarcinoma) | 1.5 |
One intraodular vessel | 2.2 |
Two intranodular vessels | 3.1 |
More than two intranodular vessels | 25.2 |
Average CT attenuation | 1.5 |
Other radiologic factors included heterogeneous density (OR, 2.5), spiculation (OR, 1.7), lobulation (OR, 1.5), pleural retraction (OR, 1.4), bubble lucency (OR, 1.8), and air bronchogram (OR, 1.7).
The radiologic ternary classification model developed by the investigators achieved an excellent overall diagnostic performance with a C index of 0.92. Using average diameter alone yielded a C index of 0.86, while adding average CT attenuation to the average size improved performance with a C index of 0.89 (both p < 0.001 compared with ternary model).
They called for future research to focus on multi-institutional studies with external validation and prospective clinical trial with long-term follow-up data, adding that this approach should be applied to a screening population of non-Asian cohorts and that AI could help further improve predictive performance.
Despite the results, this approach communicates probability rather than certainty, according to an editorial written by Yuki Arita, MD, PhD, from Keio University in Tokyo, Japan, and Steven Schalekamp, MD, PhD, from the Radboud University Medical Center in Nijmegen, the Netherlands.
Arita and Schalekamp wrote that this CT-based framework should inform but not dictate individualized care. They also cautioned that treating model-derived categories as automatic triggers for intervention “risks overdiagnosis and unnecessary biopsy or resection.”
“Until models such as the one in this study are prospectively validated and locally calibrated, they are best used as decision-support tools that sharpen judgment, promote consistency, and keep our focus on the biologic outcomes that matter most to patients,” the editorial authors wrote.
Read the full study here.