Adding endovascular recanalization (ER) does not improve treatment of symptomatic nonacute intracranial artery occlusion (sNAIAO), according to research published January 6 in Radiology.
A team led by Lei Li, MD, from Beijing Tiantan Hospital in China found that medical treatment alone led to better clinical outcomes compared with CT-guided endovascular recanalization plus medical treatment. This included higher rates of adverse events with the combined treatment approach.
“The observed higher event rate in the endovascular recanalization group suggested potential procedure-related risks,” Li and colleagues wrote.
Endovascular treatment is effective for patients with acute intracranial artery occlusion -- one of the leading causes of stroke -- occurring within 24 hours of symptom onset. However, endovascular recanalization cannot be performed within the 24-hour therapeutic window in cases of sNAIAO.
Prior reports suggest that even after standard medical treatment, sNAIAO is still tied to increased recurrence risk of ischemic stroke and adverse functional outcomes. This is due to cerebral hemodynamic insufficiency. But previous retrospective studies also highlight that endovascular recanalization is feasible and promising as a therapeutic option.
Li and co-authors led a multicenter, prospective cohort study comparing clinical outcomes after endovascular recanalization plus medical treatment versus medical treatment alone in patients with sNAIAO. All procedures were conducted under general anesthesia by experienced interventional neuroradiologists with between eight and 19 years of experience.
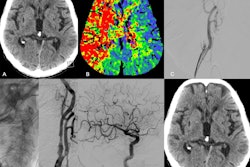
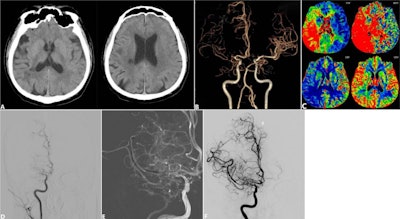 Images depict a 54-year-old male patient with nonacute right middle cerebral artery occlusion show anterior circulation symptomatic nonacute intracranial artery occlusion at imaging screening and endovascular recanalization. (A) Axial non-contrast CT images show infarction in the right middle cerebral artery territory with an Alberta Stroke Program Early CT score of 8. (B) CT angiographic image shows occlusion of the right middle cerebral artery. (C) Axial CT perfusion images show hypoperfusion in the right middle cerebral artery territory. (D) Baseline angiography confirmed right middle cerebral artery occlusion with an American Society of Intervention and Therapeutic Neuroradiology/Society of Interventional Radiology collateral grade of 2. (E) Intraprocedural angiography showed balloon angioplasty being performed at the occluded segment. (F) Postprocedural angiography demonstrated successful recanalization of the occluded artery after balloon angioplasty (Expanded Treatment in Cerebral Infarction, known as eTICI, grade 3 with residual stenosis of 30%), and thus no stent was used.RSNA
Images depict a 54-year-old male patient with nonacute right middle cerebral artery occlusion show anterior circulation symptomatic nonacute intracranial artery occlusion at imaging screening and endovascular recanalization. (A) Axial non-contrast CT images show infarction in the right middle cerebral artery territory with an Alberta Stroke Program Early CT score of 8. (B) CT angiographic image shows occlusion of the right middle cerebral artery. (C) Axial CT perfusion images show hypoperfusion in the right middle cerebral artery territory. (D) Baseline angiography confirmed right middle cerebral artery occlusion with an American Society of Intervention and Therapeutic Neuroradiology/Society of Interventional Radiology collateral grade of 2. (E) Intraprocedural angiography showed balloon angioplasty being performed at the occluded segment. (F) Postprocedural angiography demonstrated successful recanalization of the occluded artery after balloon angioplasty (Expanded Treatment in Cerebral Infarction, known as eTICI, grade 3 with residual stenosis of 30%), and thus no stent was used.RSNA
Final analysis included 436 participants with a median age of 57. Of the total, 288 underwent medical treatment alone, and 148 underwent endovascular recanalization plus medical treatment. The researchers used both CT angiography and digital subtraction angiography images for diagnosis.
The team labeled the primary outcome as “a composite of any stroke or death within 30 days after enrollment or ischemic stroke in the same region as the qualifying artery between 30 days and one year after enrollment.”
Compared with medical treatment alone, ER plus medical treatment increased the incidence of the primary outcome (adjusted hazard ratio [aHR], 2.8; p < 0.001). Within 30 days of enrollment, the risk of stroke or death was greater in the combined treatment group than in the medical treatment-only group (aHR, 21.74; p < 0.001).
The team reported no evidence of a difference between both groups in the incidence of ischemic stroke in the territory of the qualifying artery (aHR, 0.62; p = 0.33) between 30 days and one year after enrollment.
The results point to sNAIAO as a “distinct and higher-risk entity” for endovascular treatment compared with intracranial artery stenosis, the study authors wrote. They added that this needs specific procedural refinements and refined patient selection criteria in future research.
“Given the limitations of our study, the findings should be interpreted as hypothesis-generating and warrant validation in high-quality, prospective randomized controlled trials,” the authors wrote.
The study adds to the current body of limited evidence on best practices for managing patients with sNAIAO, according to an accompanying editorial written by Neeraj Chaudhary, MD, and Zachary Wilseck, MD, from the University of Michigan.
The two added that the results "should help pave the way for future prospective randomized controlled trials when better patient selection tools are more established."
Read the full study here.