CT and MRI analysis support the benefits of an emerging embolization procedure for treating chronic subdural hematoma, according to a study published January 27 in Radiology.
The procedure was shown to improve outcomes for patients in a recent clinical trial (EMBOLISE trial), with researchers now providing imaging metrics that describe how the intervention changes hematomas over time.
“The clinical benefits of adjunctive middle meningeal artery embolization (MMAE) are reflected in radiologic outcomes, including lower chronic subdural hematoma volumes at follow-up imaging, supporting MMAE alongside surgery for managing [hematomas],” wrote lead author Helge Kniep, MD, of University Medical Center Hamburg-Eppendorf in Germany, and colleagues.
Chronic subdural hematoma (cSDH) -- a slow-bleeding blood clot forming between the surface of the brain and the dura -- is treated by surgery, yet many patients experience recurrence or progression and require repeat surgery, the authors explained. The recent EMBOLISE trial showed that adjunctive MMAE reduced the 90-day rate of repeat surgery from approximately 11% to 4%, they noted.
In this post hoc analysis of the EMBOLISE trial data, the researchers extended the assessment to 180 days and included absolute CT and MRI hematoma metrics. The trial assigned adults with symptomatic subacute or cSDH and an indication for surgery to surgery alone or surgery plus adjunctive MMAE with a liquid embolic agent. It included 352 participants (mean age, 72; 256 men) with a mean cSDH volume of 126 mL at screening, based on CT and/or MRI.
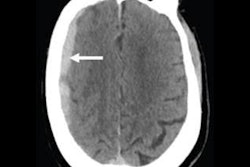
 An image demonstrating manual subdural hematoma segmentation and volume calculation.RSNA
An image demonstrating manual subdural hematoma segmentation and volume calculation.RSNA
Adjunctive MMAE resulted in lower hematoma volumes at CT and/or MRI at 90 days (20.6 mL vs. 28.9 mL; p = 0.03) and 180 days (19.4 mL vs. 31.5 mL; p = 0.04) compared with surgery alone.
Confounder-adjusted mixed-effects models confirmed a 6.9 mL (approximately 25%) greater volume reduction and 8.4 mL (approximately 30%) lower absolute volume at 90 days with MMAE versus surgery alone.
“These findings suggest that MMAE has a positive effect on long-term radiologic outcomes, supporting its use alongside surgery for managing cSDH,” the group noted.
The results warrant further large-scale studies and individual patient meta-analyses with standardized imaging outcomes to further evaluate the efficacy of MMAE as part of a therapeutic strategy for cSDHs, the researchers wrote.
In an accompanying editorial, Shakthi Kumaran Ramasamy, MD, of the Miami Cardiac and Vascular Institute in Kendall, FL, and Amanda Baker, MD, of Montefiore Medical Center in New York City, noted that MMAE has rapidly transitioned from an experimental technique to an evidence-based adjunct supported by multiple randomized trials.
“The imaging analysis from EMBOLISE shows that the clinical benefit is reflected by a measurable reduction in hematoma burden and mass effect at CT and MRI over time,” they wrote.
By refining how imaging endpoints are defined and measured, the study improves evaluation of MMAE for cSDH and supports translation of trial results into routine clinical care, Ramasamy and Baker concluded.
The full study is available here.