Ultralow-dose (ULD) photon-counting CT (PCCT) offers accurate visual and automated evaluations of emphysema at a lower radiation dose compared with low-dose (LD) PCCT -- without negatively affecting image quality, researchers have reported.
The study results support the use of ULD PCCT for this indication, wrote a team led by Qianqian Yuan, MD, of First Affiliated Hospital of Zhengzhou University in Zhengzhou, China. The group's findings were published on January 20 in Radiology.
"[Our research showed that the] radiation dose [for ULD PCCT] was reduced by 87% compared with LD PCCT, to an effective dose of only 0.2 mSv, equivalent to two standard chest radiographs," the group noted.
For patients with emphysema who undergo repeat CT imaging to monitor the disease, it's crucial to reduce radiation dose without compromising image quality or diagnostic accuracy, the authors explained. They evaluated the accuracy of ULD PCCT for both visually and quantitatively evaluating the condition, comparing ULD scans to LD ones via a study that included 152 patients with emphysema who underwent same-day LD and ULD PCCT between November 2024 and February 2025.
Two radiologists used a Likert scale to evaluate the images for the following quality measures -- overall image quality, sharpness, artifacts, and noise -- and to visually assess the subtype and severity of patients' emphysema. The investigators also included an automated emphysema quantification using low-attenuation volume (LAV) analysis in the study, converting LAV measurements to severity grades and comparing them with visual severity grades for centrilobular emphysema.
Yuan and colleagues found the following:
- The ultralow-dose protocol reduced radiation exposure by 87% compared with the low-dose protocol, with a mean effective dose of 0.2 mSv compared with 1.58 mSv (p < 0.001).
- There was no evidence of difference between the two protocols in overall image quality (median score, 4 for both [p = 0.16]); sharpness (median score, 4 for both [p = 0.08]); or artifacts (median score, 4 for both [p = 0.39]).
- They did find that ULD images were noisier than LD images, with a median score of 3 compared with 4, respectively (p < 0.001).
- Agreement was excellent between the two protocols for grading of visual centrilobular emphysema severity (weighted kappa = 0.98) and paraseptal emphysema severity (kappa = 0.96).
- The two protocols demonstrated excellent agreement in low-attenuation volume measurements across the lungs and for individual lung lobes, with intraclass correlation coefficients ranging from 0.96 to 0.98.
- Visual centrilobular emphysema severity grades showed good agreement with low-attenuation volume measurements for both the LD (weighted kappa = 0.73) and ULD (weighted kappa = 0.75) protocols.
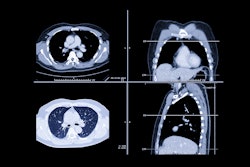
 Visual assessment of centrilobular emphysema (CLE) severity on representative axial chest CT images (window width, 700 HU; window level, -750 HU) obtained with low-dose (LD) (left) and ultra-low-dose (ULD) (right) protocols at inspiration in participants with chronic obstructive pulmonary disease. (A) LD and (B) ULD images in a 69-year-old woman. Readers categorized the participant as having trace CLE (lucencies occupying < 0.5% of the most severely affected lung zone) for both scans. (C) LD and (D) ULD images in a 74-year-old man. Readers categorized the participant as having mild CLE (lucencies occupying 0.5% to 5% of the most severely affected lung zone) for both scans.Images and caption courtesy of the RSNA.
Visual assessment of centrilobular emphysema (CLE) severity on representative axial chest CT images (window width, 700 HU; window level, -750 HU) obtained with low-dose (LD) (left) and ultra-low-dose (ULD) (right) protocols at inspiration in participants with chronic obstructive pulmonary disease. (A) LD and (B) ULD images in a 69-year-old woman. Readers categorized the participant as having trace CLE (lucencies occupying < 0.5% of the most severely affected lung zone) for both scans. (C) LD and (D) ULD images in a 74-year-old man. Readers categorized the participant as having mild CLE (lucencies occupying 0.5% to 5% of the most severely affected lung zone) for both scans.Images and caption courtesy of the RSNA.
 (E) LD and (F) ULD images in an 83-year-old man. Readers categorized the participant as having moderate CLE (lucencies occupying >5% of the most severely affected lung zone) for both scans. (G) LD and (H) ULD images in an 83-year-old man. Readers categorized the participant as having confluent CLE for both scans. (I) LD and (J) ULD images in a 61-year-old man. Readers categorized the participant as having advanced destructive CLE for both scans.Images and caption courtesy of the RSNA.
(E) LD and (F) ULD images in an 83-year-old man. Readers categorized the participant as having moderate CLE (lucencies occupying >5% of the most severely affected lung zone) for both scans. (G) LD and (H) ULD images in an 83-year-old man. Readers categorized the participant as having confluent CLE for both scans. (I) LD and (J) ULD images in a 61-year-old man. Readers categorized the participant as having advanced destructive CLE for both scans.Images and caption courtesy of the RSNA.
"[The use of ULD PCCT] may serve as a valuable tool for emphysema diagnosis and for evaluation and long-term follow-up in patients with chronic obstructive pulmonary disease," the authors concluded.
Access the full article here.