Pulmonary nodule prevalence on CT is about the same in middle-aged populations regardless of smoking history, according to research published January 27 in Radiology.
A team led by Karen Sörensen, MD, from Umeå University in Sweden, also found that nodules are tied to lung disease, reticulation, and bronchiectasis in people who reported never having smoked.
“Given the observed pulmonary nodule prevalence also among those who never smoked and the association with preexisting lung conditions, it is critical to refine risk stratification models to differentiate benign from malignant nodules more effectively,” the Sörensen team wrote.
Despite their presence on CT imaging, interpreting radiologists struggle to differentiate benign from malignant nodules. Recurring CT exams and invasive procedures are often needed in follow-up analysis.
While lung cancer screening with low-dose CT (LDCT) can reduce lung cancer-specific mortality, pulmonary nodules are incidental findings when patients undergo CT for other reasons.
Sörensen and co-authors studied the prevalence of pulmonary nodules in a middle-aged population and risk factors linked to these nodules. They used secondary data from the Swedish Cardiopulmonary Bioimage Study (SCAPIS), which took place between 2013 and 2018.
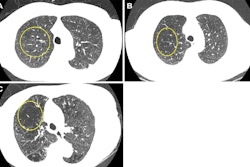
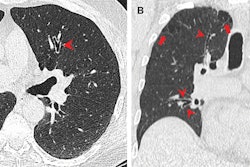
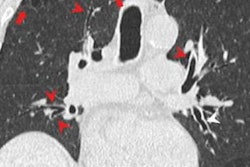
 Transverse CT images show (A) a 120-mm3 solid pulmonary nodule, marked with a circle, in the right lower lobe in a 65-year-old male; (B) a 9-mm subsolid (part solid) nodule, marked with a circle, in the left lower lobe of a 57-year-old female; and (C) a 10-mm ground-glass nodule, marked with a circle, in the left lower lobe in a 52-year-old female.RSNA
Transverse CT images show (A) a 120-mm3 solid pulmonary nodule, marked with a circle, in the right lower lobe in a 65-year-old male; (B) a 9-mm subsolid (part solid) nodule, marked with a circle, in the left lower lobe of a 57-year-old female; and (C) a 10-mm ground-glass nodule, marked with a circle, in the left lower lobe in a 52-year-old female.RSNA
Final analysis included data collected from 29,574 study participants with a median age of 57.4 years. The researchers found solid nodules sized 100 mm3 to 300 mm3 in 1,420 participants, part-solid nodules in 199 participants, and ground-glass nodules in 430 participants.
The team also reported the following respective prevalences of solid nodules among participants: never smoked, 32.5%; formerly smoked, 34.5%; and currently smoke, 37.9%.
Solid nodules sized 100 mm3 to 300 mm3 showed associations with several risk factors. These included current smoking (prevalence ratio [PR], 1.38), chronic obstructive pulmonary disease (PR, 1.72), occupational exposure (PR, 1.31), emphysema (PR, 1.56), reticulation (PR, 1.96), and bronchiectasis (PR, 2.03).
Finally, the team reported positive associations between participants who never smoked and the following factors: solid nodules at least 100 mm3 and reticulation (PR, 2.28); reported lung disease other than asthma or chronic obstructive pulmonary disease (PR, 2.26); and bronchiectasis (PR, 2.17).
“Most pulmonary nodules detected were small, with only 6.1% requiring follow-up,” the researchers noted.
The study authors highlighted that large-scale population-based studies, such as SCAPIS and ongoing follow-up studies, “provide valuable insights” into the prevalence of pulmonary nodule and associations with different risk factors.
“This information is of importance in guiding clinical decision-making and optimizing follow-up strategies regardless of smoking status,” they wrote.
Read the full study here.