Emphysema found on baseline low-dose chest CT (LDCT) is tied to death related to all causes, chronic obstructive pulmonary disease (COPD), and cardiovascular disease, suggest findings published September 9 in Radiology.
Researchers led by Jessica González Gutiérrez, PhD, from the Carlos III Health Institute in Madrid, Spain, reported that previous smokers have a higher likelihood of death related to LDCT findings in a 25-year follow-up study of more than 9,000 asymptomatic adults.
“These findings highlight the clinical relevance of CT-diagnosed emphysema and its potential role in prompting earlier preventive measures for major causes of death,” Gutiérrez and colleagues wrote.
With more focus on developing comprehensive heart and lung screening, assessing emphysema has become more relevant. However, the researchers pointed out a lack of data on the prognostic value of baseline visual emphysema scoring at LDCT among people eligible for lung cancer screening.
The Gutiérrez team studied whether a single visual emphysema score at baseline LDCT is predictive of 25-year mortality from all causes, COPD, and cardiovascular disease. It used a simplified visual scoring system based on interpretations from four experienced chest radiologists.
Researchers from Weill Cornell Medical College and Mount Sinai School of Medicine in New York, as well as the University of Navarra in Spain, developed the scoring system, which showed good reproducibility and early prognostic value in a previous study (a score of 0 indicates no emphysema, while 3 points indicates severe emphysema). Researchers from both New York-based schools and the Phoenix Veterans Affairs Health Care System in Arizona also took part in the current study.
The work included 9,047 asymptomatic adults ages 40 to 85 with a history of smoking. The participants underwent baseline LDCT between 2000 and 2008. Follow-up continued until death, follow-up drop off, or the end of the study period on December 31, 2024.
The participants had a median of 43 pack-years for smoking, and 2,637 (29.1%) had emphysema. Of those who had emphysema, 1,908 (21.1%) had mild cases, 512 (5.7%) had moderate cases, and 217 (2.4%) had severe cases. The researchers also reported a median follow-up of 23.3 years.
They found that emphysema is independently predictive of all-cause mortality (hazard ratio [HR], 1.29; p < 0.001), COPD mortality (HR, 3.29; p < 0.001), and cardiovascular disease mortality (HR, 1.14; p = 0.04). The team also observed a dose-response relationship between emphysema severity and both all-cause and COPD mortality, but not cardiovascular disease mortality.
In the adjusted competing risk analysis, emphysema remained tied to COPD mortality (HR, 3.06; p < 0.001). However, this did not go for cardiovascular disease mortality (HR, 1.04; p = 0.59).
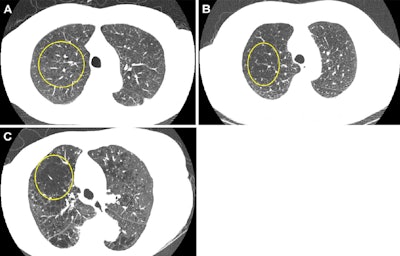 Representative axial images of mild, moderate, and severe emphysema at baseline low-dose CT (LDCT). Participants were categorized as having no emphysema or mild, moderate, or severe emphysema. When present, emphysema was mild if no distinct regions of reduced attenuation were visible on the CT scan, but vascular splaying indicates parenchymal expansion, or if only occasional discrete low-attenuation regions were observed. Moderate emphysema was defined by the presence of identifiable low-attenuation regions affecting less than half of the lung parenchyma, whereas severe emphysema was defined by the presence of identifiable low-attenuation regions that involved more than half of the lung parenchyma. A scoring system from 0 to 3 was applied, corresponding to none, mild, moderate, and severe emphysema, respectively. Yellow circle indicates the extent of emphysema. (A) A 67-year-old man with mild emphysema at baseline LDCT in 2002. Baseline LDCT scan shows vascular splaying, suggesting parenchymal expansion due to emphysema and occasional discrete low-attenuation regions. The participant ultimately died of cardiovascular disease 15.4 years (184.2 months) later. (B) A 69-year-old man with moderate emphysema at baseline LDCT in 2007. The participant died of cardiovascular disease 1.8 years (21.9 months) later. Identifiable low-attenuation regions affected less than half of the lung parenchyma. (C) An 85-year-old woman with severe emphysema at baseline LDCT in 2006. After 5.5 years (65.5 months) of follow-up, the participant died due to chronic obstructive pulmonary disease–related causes. Identifiable low-attenuation regions involved more than half of the lung parenchyma.Image and caption courtesy of the RSNA.
Representative axial images of mild, moderate, and severe emphysema at baseline low-dose CT (LDCT). Participants were categorized as having no emphysema or mild, moderate, or severe emphysema. When present, emphysema was mild if no distinct regions of reduced attenuation were visible on the CT scan, but vascular splaying indicates parenchymal expansion, or if only occasional discrete low-attenuation regions were observed. Moderate emphysema was defined by the presence of identifiable low-attenuation regions affecting less than half of the lung parenchyma, whereas severe emphysema was defined by the presence of identifiable low-attenuation regions that involved more than half of the lung parenchyma. A scoring system from 0 to 3 was applied, corresponding to none, mild, moderate, and severe emphysema, respectively. Yellow circle indicates the extent of emphysema. (A) A 67-year-old man with mild emphysema at baseline LDCT in 2002. Baseline LDCT scan shows vascular splaying, suggesting parenchymal expansion due to emphysema and occasional discrete low-attenuation regions. The participant ultimately died of cardiovascular disease 15.4 years (184.2 months) later. (B) A 69-year-old man with moderate emphysema at baseline LDCT in 2007. The participant died of cardiovascular disease 1.8 years (21.9 months) later. Identifiable low-attenuation regions affected less than half of the lung parenchyma. (C) An 85-year-old woman with severe emphysema at baseline LDCT in 2006. After 5.5 years (65.5 months) of follow-up, the participant died due to chronic obstructive pulmonary disease–related causes. Identifiable low-attenuation regions involved more than half of the lung parenchyma.Image and caption courtesy of the RSNA.
The study authors wrote that since both emphysema and coronary artery calcification stem from smoking, future research on how these conditions progress may give further insights into their interaction. This information could also influence risk stratification for cardiovascular disease and COPD. The authors suggested that AI could help in this area.
“Clinically, these findings suggest emphysema is not merely an incidental CT finding but a distinct disease entity associated with worse outcomes and increased mortality, not only from lung cancer but also from respiratory and [cardiovascular disease] deaths,” they wrote.
Read the full study here.