An article in the January issue of the Journal of the American College of Radiology offers expert advice on radiation dose optimization techniques in pediatric CT. What's the most important step? Making sure a pediatric CT study is justified before it even begins, according to the authors.
Between 7 million and 8 million CT examinations are performed for various pediatric clinical indications per year in the U.S., a figure that merits particular attention due to the higher susceptibility of children to radiation-related risks than adults, and because of their higher organ radiosensitivity and longer expected life spans.
Justifying the scan is the radiologist's most important job, inasmuch as a substantial number of CT scans are unnecessary, and similar information can often be obtained from radiography, ultrasound, or MRI, according to lead author Dr. Sarabjeet Singh and colleagues from Massachusetts General Hospital (MGH) (JACR, January 2012, Vol. 9:1, pp. 77-79).
Web-based computerized radiology order-entry systems, which use clinical decision-support rules governed by appropriateness guidelines such as the American College of Radiology Appropriateness Criteria, are a key step in justifying exams, Singh and colleagues wrote.
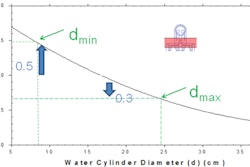
Understanding the body region to be imaged -- for example, knowing when intrinsically higher contrast, such as in the lungs, permits lower doses -- can help optimize protocols. Most pediatric CT exams for bone conditions, such as chest CT for pectus deformities, whole-spine CT for scoliosis evaluation, or extremity CT for bone trauma, can be performed at the lowest allowed fixed-tube currents, the authors wrote.
Protocols for every body region should be designed for stratified dose reduction based on the clinical indication. On the other hand, higher image noise in head CT can interfere with visualization of gray- and white-matter differentiation of the cortical region, so MGH generally limits head CT scans to lower-dose shunt patency, bony skull, and intracranial hemorrhage scans. In addition, localizer radiographs and tube current and tube voltage optimization can substantially reduce radiation doses.
When using second-generation dual-source CT scanners, a very high nonoverlapping pitch (up to 1.6:1 to 3.4:1) combined with table speeds as fast as 450 mm/sec permit fast scanning with few motion artifacts and substantial radiation dose savings, Singh and colleagues wrote. Finally, minimizing scan length, as well as using image-processing techniques such as iterative reconstruction, can reduce doses by as much as 30%.
Because of children's higher sensitivity to radiation, it's crucial to keep clinical indications, patient weight, and any prior imaging exams available to optimize the radiation dose, the authors concluded. More information is available at imagegently.org.