When ordering neck CT exams, do pediatricians know the potential risk of thyroid cancer to their patients from exposure to radiation scatter? Are parents adequately informed? Are they given accurate risk incidence data?
These questions weren't answered at a scientific session at the 2010 RSNA meeting about pediatric dose reduction and the Image Gently initiative. But they were clearly on attendees' minds during a presentation explaining how to estimate radiation dose exposure to the thyroid and the corresponding cancer risks for children having a neck CT scan.
The risk to children of developing thyroid cancer is not uniform, explained Walter Huda, PhD, a medical physicist and professor of radiology at the Medical University of South Carolina (MUSC) in Charleston. It is a factor of sex, age, body mass size, and, of course, radiation dose. Calculating an individual patient's risk based on specific radiation doses is essential, because using a pediatric anthropomorphic phantom CT will not produce accurate information.
Huda and colleagues estimated radiation dose to the thyroids of 80 consecutive patients who underwent neck CT exams, and then calculated cancer risk. The patients ranged in age from neonates through 18 years.
The MUSC researchers determined that the risk of developing thyroid cancer is seven times higher for girls than for boys. The risk for 12-month-old male infants is four times higher than for 16-year-old boys. For 12-month-old girls, the risk is double: eight times higher than for 16-year-old girls.
"This information is important because an exam's diagnostic benefit should exceed the corresponding cancer risk from radiation exposure," Huda said. "If you don't know what your patient's risk aspect actually is, it is not clear to me how you would figure out if this is an indicated exam."
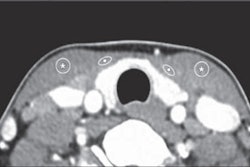
The research team obtained data on the sex, age, and average CT dose index volume (CTDIvol) used to perform the CT exam for each patient. CTDIvol data were used to estimate the corresponding thyroid dose in the mathematical anthropomorphic phantom used in the ImPACT CT Patient Dosimetry Calculator. The researchers obtained patient doses by modeling the patient and phantom neck regions as mass-equivalent water cylinders (average diameter, 14 ± 4 cm) and using a patient size-dependent correction factor.
The average thyroid dose estimates were 28 mGy for boys and 32 mGy for girls. Mean thyroid doses were 37 mGy for infants and 30 mGy for teenagers, Huda said. The thyroid cancer risk for males was 0.02%, on average, and the risk for females was 0.14%.
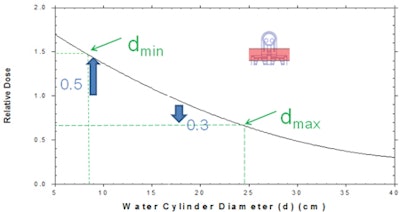
"The mathematical anthropomorphic phantom has a neck diameter that is 16.5 cm," he said. "Our smallest patient had a neck diameter of approximately 10 cm and our largest patient had a neck diameter of nearly 25 cm. With this cohort, the patient's average neck size was about 14 cm. If we had used a constant CT exposure based on the neck size of the phantom, estimated thyroid doses would have been 17% lower for our average-sized patient."
"What I would like to point out is that if you simply multiply your clinical CTDIvol, you are obtaining the dose to this particular phantom," he said. "You don't get your patient's organ dose."
Calculating dose
MUSC takes into account the actual size of the patient, which can be readily obtained from the CT images. For each slice, medical physicists know the area of the patient, and the average Hounsfield unit that permits them to estimate the mass of the patient being irradiated.
They then compare the mass of the patient with the corresponding mass of the phantom used in the ImPACT dosimetry calculator. Once they know the two sizes, they utilize published data (Huda et al, 1997, Radiology, Vol. 203:2, pp. 417-422) that tells them how dose varies with size. These data permit the production of a dose correction factor for each patient that explicitly takes into account the patient's physical characteristics. If the patient is larger than the phantom, doses will be reduced and vice versa.
Once the thyroid radiation dose for a patient has been determined, these organ doses are converted into a corresponding risk of thyroid cancer induction using risk data published by the National Academy of Sciences' Biological Effects of Ionizing Radiation (BEIR) VII in 2005. As is well-known, these risk factors all depend on the patient's age and sex.
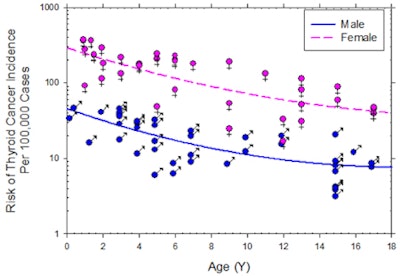 |
| Thyroid cancer risk: age and sex dependent. Image courtesy of Walter Huda, PhD |
Radiologists' advice to physicians
Huda emphasized that his responsibilities as a medical physicist should be limited to providing accurate estimates of radiation dose and cancer risk for any diagnostic imaging exam. The responsibility of determining the appropriateness of a CT scan should be made by the ordering clinician and by radiologists.
What happens when a radiologist disagrees with a pediatrician's order? Who should inform parents of the cancer risk of a diagnostic imaging exam: the ordering physician or a radiologist? Huda deferred to his colleagues and radiologists in attendance to provide these answers.
In a subsequent e-mail to AuntMinnie.com, lead author M. Vittoria Spampinato, MD, assistant professor of neuroradiology, wrote: "At MUSC, a radiologist evaluates the indication of a neck CT in a pediatric patient and determines on a case-by-case basis whether the benefit of the study outweighs the risk. If the study is not warranted, we do contact the referring physician to further discuss the study indication."
The MUSC radiology department does not formally discuss the risks of particular exams being ordered with patients, according to Spampinato.
By Cynthia E. Keen
AuntMinnie.com staff writer
December 24, 2010
Related Reading
Radiation ups pediatric thyroid risk, December 17, 2010
Radiologists expand proactive dose safety efforts, December 2, 2010
One-quarter of outpatient CT and MRI exams are inappropriate, March 1, 2010
Studies spotlight high CT radiation dose, increased cancer risk, December 14, 2009
Risk of thyroid cancer increased in childhood cancer, October 28, 2009
Copyright © 2010 AuntMinnie.com