Routine CT lung cancer screening of high-risk individuals would save thousands of lives per year for less than a dollar a month per patient if it were implemented throughout the U.S. -- and would be even cheaper than breast screening, concludes a new study in the April issue of Health Affairs.
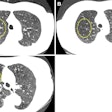
Lung cancer is one of the deadliest cancers on the planet, claiming more than 150,000 lives per year in the U.S. alone. In recent years, however, several studies of using low-dose spiral CT to screen asymptomatic people at high risk of lung cancer has found that screening can detect early-stage disease. In particular, the 2010 National Lung Screening Trial (NLST) found that three annual rounds of routine CT screening in high-risk populations would reduce mortality by at least 20%.
Despite these findings, widespread screening has yet to be implemented in the U.S., in part due to cost concerns. But this week's new study finds that screening costs are minimal when spread out over large numbers of policy holders in a high-risk population of smokers and former smokers. Investigators found that the cost of adding CT screening would be less than $1 per month for holders of commercial healthcare insurance plans, far cheaper than breast cancer screening at about $3 a month (Health Affairs, April 2012, Vol. 31:4, pp. 770-779).
Accumulating evidence
"The evidence of the value of advanced screening technology for lung cancer has accumulated to the point where we can show very strong cost-effectiveness for the commercial population," said lead author Bruce Pyenson, a consulting actuary at Milliman, in a statement accompanying the study's release. "Late stage lung cancer is deadly, but if treated at an early stage, survival is very good. That's what makes early detection so promising."
The management of screen-detected lung cancer continues to improve, with both CT scanning and surgical techniques evolving rapidly, Pyenson and colleagues wrote. Currently, early-stage lung cancer can usually be cured with surgical removal of the tumor alone. However, future improvements in lung cancer surgery might further reduce the risks and costs associated with surgical intervention, and potential money-saving measures were modeled into some of the study's different screening-cost scenarios.
The study estimated the cost and benefit of lung cancer screening in the high-risk U.S. population who had private commercial health insurance, wrote Milliman et al. The model consisted of two sequential steps: first determining the costs of screening to commercial payors, such as insurers and health maintenance organizations, then performing a cost-benefit analysis to calculate how many life-years could be saved with screening via early detection and treatment.
The model was designed to estimate cost-benefit of lung cancer screening for U.S. smokers and former smokers between the ages of 50 and 64 with a history of at least 30 pack-years of smoking -- a group representing about 18 million people in the U.S. (A pack-year is defined as smoking one pack of cigarettes each day for one year.) The authors applied actuarial methods that are commonly applied to new insurance offerings.
Screening methods were based on published annual protocols for both low-dose spiral CT lung cancer screening and follow-up visits within the first year after the baseline scan until the patient was diagnosed with cancer or determined to be cancer-free, the authors wrote. All patients received an initial screening and annual repeat screenings. Costs were based on the 2011 national Medicare Physician Fee Schedule for most services, which might include an additional CT scan or biopsy of a suspicious lung nodule. Also included in the cost assumptions was 30 minutes of smoking-cessation counseling with each screening.
"Based on published data, initial low-dose spiral CT screenings of patients produce results that require near-term diagnostic evaluation 21% of the time, whereas repeat annual screening requires near-term diagnostic evaluation 7% of the time," Pyenson and colleagues explained. The group used near-term diagnostic evaluation rates that were about 50% and 30% higher, respectively, than the published rates to allow for worse-than-reported performance of the screening.
The heart of the cost-benefit calculation was a stage-shift model in which intervention in the form of screening shifted the distribution of cancer stages back by two years toward earlier, more curable disease, they said, leading to lower treatment costs, and more people cured of cancer more cost-effectively. These data were then compared to a status quo scenario in which cancers were distributed using historical stages, costs, and mortality. The study assumed that 100% of the target population was screened each year, and that this population would generate 90% of the cancer cases.
To pay for the screenings, the model assumed that 50% of the target population would accept a lung cancer insurance screening rider at a reimbursement level equivalent to that of colorectal cancer screening.
Many lives, saved cheaply
The study estimated that the average annual cost of lung cancer screening was $247 per person screened, based on assumptions that 75% percent of the screenings were repeat procedures, which is consistent with published literature. The price of repeat screening plus follow-up was estimated at one-third lower than that of initial screening, because the repeat exam is less comprehensive. Assuming that half of the target population between the ages of 50 and 64 were screened, the insurer cost spread across the commercial population would be 76 cents per member per month with no cost sharing, the study team found.
"Assuming current commercial reimbursement rates for treatment, we found that screening would cost about $1 per insured member per month in 2012 dollars," Pyenson et al wrote. "The cost per life-year saved would be lower than $19,000, an amount that compares favorably with screening for cervical, breast, and colorectal cancers."
The assumption that screening would not involve cost sharing is consistent with the Affordable Care Act's provision for preventive services that have a task force rating of A, for unequivocal benefit, or B, for objective benefit but some harm, the group wrote.
The baseline screening scenario would lead to more than 130,000 additional lung cancer survivors in 2012, which does not include some 64,000 "lead-time people" who would be living with mostly earlier-stage lung cancers who became symptomatic within two years of screening, the group wrote. The baseline scenario assumed that screening 30% of people between the ages of 50 and 64 (about 18 million people) would capture 90% of lung cancers. Changes in costs in the table below reflect the benefits and costs assuming that screening 40% (24 million people) or 20% (12 million people) of the target population would capture 90% of lung cancers. Similarly, the three cost scenarios made different assumptions about the annual cost of treatment.
The model assumed low managed-care reimbursement for low-dose CT scans, consistent with the authors' views that lung cancer screening coverage "should be restricted to high-throughput, high-efficiency, and low-cost sites," Pyenson et al wrote.
Cheaper than other screening exams
In each of the scenarios below, lung cancer screening is cheaper than the average cost for other cancers because the target population -- smokers and former smokers -- is smaller than for other exams. In addition, "lung cancer screening has a lower cost per life-year saved than other screenings, because symptomatically detected lung cancer is frequently more quickly fatal than other cancers," they wrote. "This means that the number of life-years saved is higher."
Cost of CT lung screening versus other screening exams
|
The analysis was completed before the results of the NLST study showing a 20% mortality reduction was published. The authors' estimates of the proportion of early-stage cancers that would be detected by screening and therefore mortality reduction are more optimistic, the authors noted.
"We attribute these differences partly to the design of the trial, which required that it be terminated as soon as significant mortality differences of greater than 20% appeared, and partly to our assumptions based on the use of current, improved imaging and screening workup approaches that emerged after the trial began," Pyenson et al wrote. In addition, the study model assumes screening beginning at age 50 rather than 54 for the NLST trial, which increases screening costs but yields fewer cancers.
In people younger than 65 years, lung cancer accounts for 43,000 deaths per year, about 26% of all cases. Incidence then doubles between ages 45 and 49, and again between 60 and 64, then increases more slowly until age 79, after which it begins declining, the group noted. Ignoring treatment after age 64, the age at which most Medicare coverage begins, affected both the status quo and screening scenarios and tends to understate the cost advantages of screening, because it ignores savings after age 65.
Modeled into the low-cost scenario were cost-cutting measures, including video-assisted thoracoscopic surgery and intervention based on lung nodule volume change analysis, which measures volume growth rate, reducing the need for invasive diagnostic procedures.
"Our study suggests opportunities for the efficient implementation of lung cancer screening, which would involve insurers' selection of high-quality providers and use of 'best published practices' for managing clinical aspects of screening, along with rigorous tracking of outcomes," Pyenson and colleagues wrote. "The goal would be to ensure achievable standards for quality and cost."
The study found that both the cost of screening and the cost per life-year saved compared favorably with published rates for other cancer screenings, the group concluded.
"Our findings suggest that commercial insurers should consider lung cancer screening with low-dose spiral CT to be of substantial value in high-risk populations and should consider providing coverage that includes such screening," Pyenson et al wrote. "Further study is warranted to determine the optimal screening procedure and its use in various patient populations.