A computer-aided detection (CAD) technique for virtual colonoscopy detected hard-to-find flat colorectal polyps with equivalent sensitivity it attained for polypoid lesions in the same patients, according to researchers from Boston.
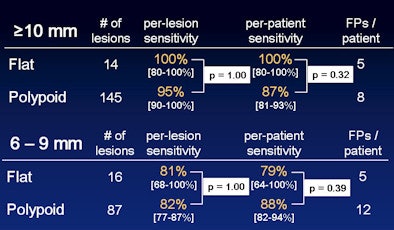
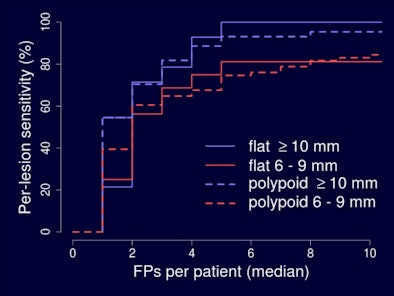
The previously validated CAD technique, applied to data from nearly 2,000 patients at 32 medical centers, achieved 100% sensitivity for flat lesions 10 mm and larger, and performed well on smaller 6-9-mm polyps.
CAD's accuracy for flat polyps was "similar for that of polypoid polyps, and lesion morphology didn't really have meaningful effect on the results," said Janne Näppi, PhD, in a presentation at the March 2012 European Congress of Radiology.
Näppi and coinvestigator Hiroyuki Yoshida, PhD, from Massachusetts General Hospital in Boston and Harvard Medical School in Cambridge, MA, collaborated on the study with data from Dr. Daniele Regge at the Institute for Cancer Research and Treatment in Turin, Italy.
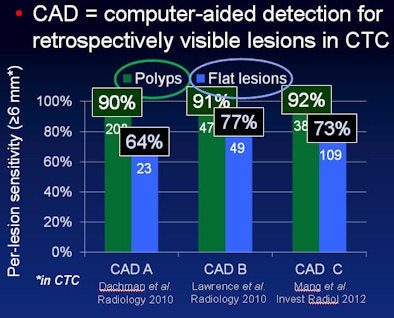
"The detection of flat lesions is known to be more challenging than that of polypoid lesions, and this is a concern because flat lesions more often have high-grade dysplasia compared to polypoid lesions," Näppi said in his talk. "CAD can be used to improve accuracy in the detection of flat lesions, but there is some concern about the detection accuracy of CAD."
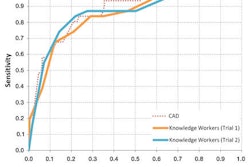
Recent studies in which several CAD schemes have logged greater than 90% accuracy for polypoid lesions scored around "80% and sometimes even closer to 60%" sensitivity in flat-lesion detection -- "and this is with as many as nine false-positives per patient," Näppi said. Finally, some previous studies have used the same training and testing datasets for the CAD systems, making true detection sensitivity difficult to evaluate.
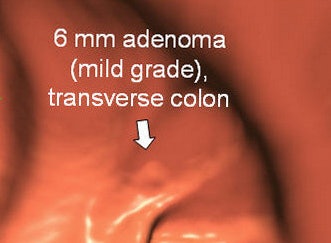
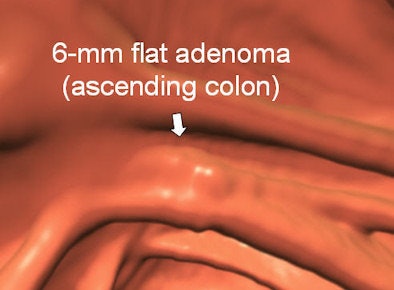
There has even been some confusion about the definition of a flat lesion, Näppi said, a category this study defined as a lesion with a vertical height < 3 mm above the surrounding normal colonic mucosa in virtual colonoscopy (also known as CT colonography, CTC).
Aiming to assess standalone flat-lesion detection in the CAD system that the investigators developed over a decade ago, the group incorporated a fully-automated CAD server incorporating independent training and testing populations from different hospitals into the detection algorithm. "Not only were the patients different in both the training and testing sets, they came from different hospitals in different geographical areas, and also the training data had been collected before the testing data," Näppi said.
The CAD scheme originally outlined in a study by Yoshida et al (IEEE Transactions on Medical Imaging, December 2001, Vol. 20:12, pp. 1261-1274), and later in a fully automated version by Näppi et al (Academic Radiology, March 2007, Vol. 14:3, pp. 287-300) was developed at the University of Chicago in Chicago and Harvard Medical School in Cambridge, MA. Since 2001 it has been refined and validated with both cathartic CTC and noncathartic CTC.
The fully automated CAD algorithm was trained on a set of studies consisting of 317 lesions, including 127 polyps 10 mm or larger and 190 polyps 6-9 mm in diameter (collected in 2000-2004 from 1,211 patients, Pickhardt et al, Rockey et al). The testing set consisted of 262 patients, including 158 polyps 10 mm or larger and 104 polyps 6 mm to 9 mm in diameter in 737 patients (collected 2004-2007, Regge et al).
In the testing population, a total of 25 patients (mean age 62 years, range 47-69 years) had flat polyps. The 25 patients had a total of 30 colonoscopy-confirmed flat lesions larger than 6 mm, 47% of which were 6 mm to 9 mm in size at colonoscopy.
According to the results, CAD detected 100% (80% to 100%) of the flat lesions 10 mm and larger, and 80% (68% to100%) of the flat lesions 6 mm to 9 mm, with a median 5 false-positive detections per dataset.
A review of the few flat lesions missed by CAD showed no specific reason why they were missed. There were clues, however, as all false negatives were 7 mm in diameter or smaller, and all were reconstructed using a wider 2.5-mm slice thickness, Näppi said. In addition, the use of fecal tagging in 28% of patients with flat lesions seemed to confer an advantage in detection sensitivity in tagged data.
"We found that detection performance was clinically acceptable," Näppi concluded. Lesion morphology had no significant effect on detection sensitivity in the study.
Session moderator Dr. Stuart Taylor from University College London asked Näppi why he thought his group's CAD performed so much better than other systems in flat-polyp detection.
"The majority of CAD systems try to identify some kind of curvature in the colon and then try to identify polyps based on this," he said. "Our CAD system establishes a thick volumetric layer around the colonic surface, and then uses a shape index feature to try to identify these lesions. For this study we didn't invent any special protocols for flat lesions, so these were our kind of conservative results."