Laxative-free virtual colonoscopy showed high sensitivity for lesion detection and an improved patient experience compared to invasive optical colonoscopy following cathartic bowel cleansing, according to results published in the May 15 Annals of Internal Medicine.
Among the largest peer-reviewed studies of reduced-prep virtual colonoscopy to date, the prospective study showed per-patient sensitivity as high as 91% for detecting lesions 10 mm or larger.
Overall detection sensitivity for virtual colonoscopy (also known as CT colonography or CTC) was lower than with the invasive optical colonoscopy studies that followed each virtual exam. However, patients reported an easier experience with VC, a factor that may encourage more eligible patients to come forward for screening.
Acceptability of the exam is a key issue in colorectal cancer screening, considering that just over half of eligible adults in the U.S. are screened for colorectal cancer. Avoidance of the laxative bowel preparation is thought to be a major reason behind their reticence.
Easier screening?
The results of the study suggest a role for CTC as an alternate and potentially more comfortable screening method that could contribute positively to overall screening participation, wrote Dr. Michael Zalis and colleagues from Massachusetts General Hospital, Brigham and Women's Hospital, and the University of California, San Francisco (Ann Intern Med, May 15, 2012, Vol. 156:10, pp. 692-702).
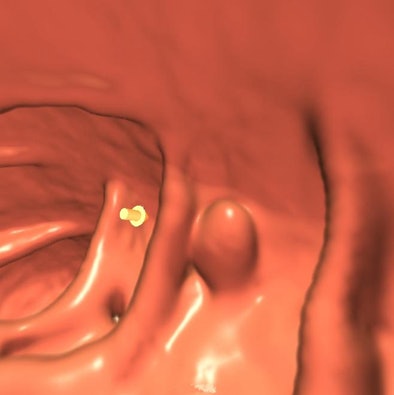 |
| 3D endoluminal view of the colon in a study patient. No laxatives were used. Yellow arrow (a computer-aided detection marker) indicates a confirmed 10-mm adenomatous polyp. Image courtesy of Dr. Michael Zalis. |
The study found "that a laxative-free CTC technique could identify patients harboring the most clinically significant polyps (those 1 cm or larger) with a performance similar to standard (laxative) CTC and optical colonoscopy," Zalis wrote in an e-mail to AuntMinnie.com. "This suggests a future role for the technique in screening."
Screening subjects have often reported a strong aversion to laxative preparations, which suggests a barrier to colorectal cancer screening that is potentially correctable and may account for relatively low screening participation, the authors wrote.
On the other hand, participants undergoing laxative-free CTC in this study "experienced a significant improvement in perceived comfort with the laxative-free preparation," Zalis said.
The study was unique not only for its size and prospective design, but also for its use of both electronic cleansing (EC) and computer-aided detection (CAD), performed using techniques developed at Massachusetts General Hospital and previously validated.
The researchers performed virtual colonoscopy followed by standard optical colonoscopy using a polyethylene glycol (PEG) prep in 606 patients. Optical colonoscopy was performed within five weeks of VC.
The cohort consisted of individuals at average and moderate risk of colorectal polyps and carcinoma. Individuals who had been screened in the previous five years, or who had risk factors such as a family history of colorectal carcinoma that could increase their risk of developing the disease, were excluded.
Preparation for the noncathartic CTC exam included fecal tagging with iodinated oral contrast (Omnipaque 300, GE Healthcare), which was administered in small aliquots for two days prior to the exam. Hydration with the patient's choice of noncaffeinated and nonalcoholic beverages was also delivered for two days prior to the exam, as was a zero-fiber meal kit (NutraPrep, Bracco Diagnostics) one day before the exam; no bowel purgative was used.
On the day of the exam, the colon was insufflated automatically (ProtoCO2l, Bracco) with CO2. No antispasmodic agents were used.
CTC was performed on 16- or 64-detector-row scanners using single-breath-hold prone and supine positioning with a low-radiation-dose protocol (120 kVp, 50 mAs effective). Detectors were configured for maximum 2.5-mm z-axis length with 1.25-mm overlap interval.
Electronic cleansing of the images was performed to virtually remove the tagged fecal material and fluid, and images were interpreted using CAD. All interpretations were performed on a single V3D workstation, version 2.1.3 (Viatronix), modified to include proprietary electronic cleansing and CAD applications.
Optical colonoscopy examinations were initially blinded to CTC results, which were subsequently revealed during colonoscope withdrawal; this method permitted re-examination to resolve discrepant findings. Unblinded optical colonoscopy served as a reference standard.
Results
For adenomas 10 mm or larger, per-patient sensitivity of CTC was 91% (95% confidence interval [CI]: 0.71-0.99) with specificity of 85% (95% CI: 0.82-0.88). The sensitivity of optical colonoscopy was 95% (95% CI: 0.77-1.00) with specificity of 89% (95% CI: 0.86-0.91).
The specificity of optical colonoscopy at the threshold of 8 mm or larger was 91% and at 6 mm or larger was 94%, compared with 86% for CTC at the threshold of 8 mm or larger and 88% at 6 mm or larger (p = 0.02).
Diagnostic accuracy by polyp size, CTC vs. optical colonoscopy (OC)
|
||||||||||||||||||||||||||||||||||||||||||
Of the confirmed lesions with advanced histology, 85% (22 of 26) were 10 mm or larger, Zalis and colleagues wrote. Of the four advanced lesions smaller than 10 mm, one showed high-grade dysplasia and three had villous features. Three cases of cancer were confirmed, all in lesions larger than 10 mm. The mean interval between CTC and optical colonoscopy was 17 days.
The overall performance for adenoma detection of laxative-free CTC was lower than that of first-pass CTC, the authors wrote. At lesion thresholds of 8 mm or larger and 6 mm or larger, the magnitude of observed differences in sensitivity on a per-patient basis was clinically significant. However, the limited size of the patient cohort and, especially, the small number of larger lesions made comparison difficult.
Restricting the study to a low-risk cohort limited the prevalence of lesions and the study's statistical power, especially for polyps 10 mm and larger, the authors wrote.
Still, "the new technique does not appear to be as accurate as standard CTC or optical colonoscopy for detecting the smaller lesions," Zalis said. "Fortunately, those lesions are also much less likely to harbor the cellular changes that indicate likely subsequent development of cancer."
Better patient experience
As for patient experience with the two exams, both comfort and difficulty of examination preparation favored virtual colonoscopy over optical colonoscopy. A total of 92.4% (559 of 605) of study participants completed a survey on comfort, reporting median scores of 1 for CTC and 2 for optical colonoscopy on a scale of 1 to 5, with 5 representing severe discomfort.
Rating bowel habit changes, also on a scale of 1 to 5, the median score was 2 for CTC and 4 for optical colonoscopy (p < 0.001 for all comparisons). Among the 77% of participants expressing a preference between CTC and optical colonoscopy for future exams, 290 preferred CTC and 175 preferred optical colonoscopy (p < 0.001).
"Patients reported a better experience with CTC examination preparation over standard, cathartic preparation," Zalis and colleagues wrote. "Readers deemed most cases adequate for interpretation, and we observed no major adverse events with either technique. These results suggest that laxative-free CTC can detect the most clinically important polyps and could contribute to colon cancer screening."
For adenomas, 74% (31 of 42) of false-negative results occurred in CTC exams with low image quality (3 or lower on a scale of 1 to 5, with 5 being optimal). Optical colonoscopy had 23 false negatives, fairly evenly distributed throughout the colon.
Previous decision modeling studies suggest that CTC is more cost-effective than no screening. In addition, CTC may be shown to be cost-effective versus optical colonoscopy if CTC is able to improve screening participation among adults 50 and older who have shied away from optical colonoscopy.
Laxative-free CTC addresses an important barrier to screening, and its potential effect on screening merits further investigation that will be needed before widespread implementation can begin, the authors stated. But the current study offers hope that virtual colonoscopy could ultimately help boost screening rates.
"Colon cancer is almost completely preventable through screening," Zalis said. "Currently, despite the fact that optical colonoscopy is an effective test, not enough people are willing or able to undergo it. Standard CTC is easier and cheaper (approximately 30% cost of optical) and is very accurate, but it, too, requires the prep that deters participation. If we could validate a more patient-friendly exam, that might help improve overall screening, especially for those folks who are not already willing to participate."




















