Dear AuntMinnie Member,
It's been a big week for CT lung screening. Hot on the heels of new guidelines calling for the screening of high-risk smokers, the question of who else should get screened has been the subject of several presentations at this week's American Thoracic Society (ATS) meeting in San Francisco.
Given that CT lung screening has been shown to produce a 20% mortality reduction in heavy smokers, should the technology also be used for those without such long smoking histories? Definitely not, according to a presentation by Dr. Gerard Silvestri on Tuesday. International editor Eric Barnes was in attendance and filed a story for our CT Digital Community.
Research has shown that CT lung screening's benefits for low-risk individuals don't outweigh the risks and costs, Dr. Silvestri said. For example, he cited one study that found that CT screening of smokers who have quit and, thus, are at lower risk can cost up to $2.3 million per quality-adjusted life year -- not a bargain by any means.
Dr. Silvestri offers his perspective on the CT lung screening debate, as well as a cautionary word on what might happen to CT screening if commercial interests win out over science in determining who should get screened. Read more by clicking here.
In another ATS presentation, researchers from the University of Pittsburgh report on their work in determining whether emphysema is a risk factor for lung cancer. They found that it is, but the results raise another intriguing question: Should individuals with emphysema get CT screening, even if they don't meet the recently released guidelines? Get more details by clicking here, or visit the community at ct.auntminnie.com.
Breast density and imaging
Meanwhile, believe it or not, there are other body parts besides the lungs making headlines these days. In breast imaging, specialists are trying to figure out how to deal with mammography of women with dense breast tissue, which is known to confound traditional x-ray-based imaging.
Other imaging modalities are available to fill the gap, such as automated breast ultrasound (ABUS) and digital breast tomosynthesis (DBT). But these technologies are new and still in the early phases of adoption.
Uptake could get a boost, however, thanks to grassroots initiatives to pass breast density notification laws, which require that women be told of their density status. Passage of the first density notification law in Connecticut led to a surge of interest in supplemental breast imaging modalities such as ultrasound.
Density notification laws in other states could spur similar spikes, and they could also help market penetration of technologies such as ABUS and DBT, according to an article in our Women's Imaging Digital Community. Learn more by clicking here.
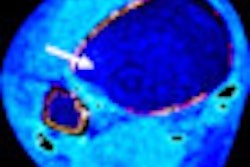
In other women's imaging news, read about a new study released this week in Radiology that found that MRI can be used to predict the effectiveness of chemotherapy. The finding could help oncologists direct treatment for the disease, according to the article, which you can read by clicking here.