The terms "low dose" and "standard dose" are meaningless, so if the paper you're submitting to Radiology includes them, expect to get it back, say the editors of the specialty's flagship journal.
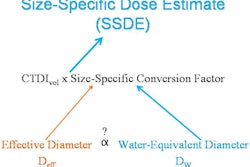
Authors should instead express dose levels in CT dose index volume (CTDIvol), dose-length product (DLP), effective diameter, and size-specific dose estimates (SSDE) -- avoiding effective dose as well, save for the broadest dose comparisons, according to Radiology editors Dr. Alexander Bankier, PhD, and Dr. Herbert Kressel.
Why use these measures instead of nebulous terms such as low dose or effective dose expressed as mSv? Because together these alternatives paint the dose picture in the context of the patient being scanned, wrote Bankier and Kressel, who also hold positions at Boston's Beth Israel Deaconess Medical Center.
CTDIvol and DLP provide information about scanner radiation output, while effective diameter offers information about the dimensions of the study participants, and SSDE provides an approximation of the dose absorbed by the individual patient, they explained. Terms such as low dose and standard dose are limited by several factors, including changing dose standards over time, geographic differences in patient care, and even differences as to what constitutes low-dose scanning between patients.
"We believe that the only remedy to these concerns is the general avoidance of the term low dose and its replacement by terminology that will allow precise and reproducible comparisons of dose between and within studies," Bankier and Kressel wrote (Radiology, October 2012, Vol. 265:1, pp. 4-8).
Low dose today is standard dose tomorrow
In the days before automatic exposure control (AEC), when the term low dose was introduced into the literature, dose calculation was a relatively straightforward process performed with single tube current settings, often 120 kV. This made dose index levels relatively easy to calculate and compare among different CT scanner models, protocols, and patients.
However, when AEC arrived on the scene, patient factors such as body habitus, circumference, and position in the CT gantry began to affect dose index values used in scans, and its use now creates problems, they explained.
In addition, the definition of low dose changes over time with the evolution of technology and practice. The efforts of radiologists, medical physicists, and manufacturers to reduce radiation dose have led to new clinical standards and practices, the development of new CT scanners, and the introduction of AEC, noise reduction algorithms, and new image reconstruction techniques. As a result, protocols that were considered low dose a decade ago are now widely accepted as clinical standards.
Take the National Lung Screening Trial (NLST) as an example. "The technical protocol of the NLST was designed in 1998, and for that time it was a real low-dose protocol ... but according to current standards it's certainly no longer a low-dose protocol, though it's still called low dose," Bankier said in an interview with AuntMinnie.com.
"So the term ages very quickly," he said, "and hopefully what we consider to be low dose today will be standard dose a few years from now, and then something else will be low dose because our efforts to develop technology such that dose to patients could be lowered is an ongoing process."
An effective dose of 1.5 mSv for CT lung cancer screening was considered low in 1998 when NLST was designed, but images are routinely acquired now at 1 mSv or less using AEC. So terms such as low dose, ultralow dose, and so on, are confusing both to patients and clinicians, he said.
The term low dose also means different things in different geographic locations -- that is, different geographic regions have different awareness and dose issues, and patient sizes also vary substantially in different regions.
"Dose measurements refer to a standard patient who has a fixed weight and a fixed height," Bankier said. "But as we know, a standard patient -- or median patient, if you want -- can look very different in the U.S., Europe, or Asia, so a standard patient could look very different depending on the country of origin."
Recognizing these differences, the World Health Organization avoids the use of fixed thresholds in favor of ranges of body mass index to define categories such as normal, overweight, or underweight, and it continuously adapts these ranges with respect to geography, the editors noted.
Finally, different regions have different histories and experience with regard to low-dose imaging, Bankier said. "For example, in Europe, we were a little ahead of the rest of the world, so regulations there are more stringent than in the rest of the world," he said. When a manuscript is reviewed with one European and one U.S. reviewer, "they understand very different things when we say low dose."
Patient context needed
For Bankier and Kressel, the solution to these concerns is to avoid the term low dose except for the most general descriptions, and replace it in every paper with terminology that enables precise and reproducible comparisons between studies with an understanding of patient parameters.
The use of effective dose, expressed in mSv, is one way to express dose, but it has several limitations owing to phantom limitations. And it represents a calculation of the relative radiosensitivity of an organ that is based not on the individual patient but on a standard patient size. The vagaries and oversimplifications inherent in this measure mean that effective dose shouldn't be used to assess risk.
"We collaborated with a number of very knowledgeable radiation physicists, and there is a broad consensus among them that effective dose should not be used," Bankier said. "It's a good method to compare general radiation between radiation technologies, but it's not a good metric to quantify patient-related radiation."
Overlapping terminology
Bankier and Kressel recommend that authors report all four dose parameters: CTDIvol, DLP, effective patient diameter, and SSDE. CTDIvol and DLP provide information about the radiation output of the scanner, effective diameter provides information about the size and dimensions of the study cohort, and SSDE provides an approximation of the dose absorbed by the individual patient for a given scan.
How did they reach this conclusion? "First, CTDIvol is the most commonly known parameter that quantifies the radiation output of a standard model, and this parameter is included in most of the dose reports that are generated by CT units," Bankier said.
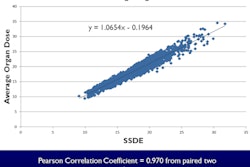
The second parameter, DLP, gives additional information about the scan length (DLP = scan length x CTDIvol), he said. The effective diameter works only for the torso, but it quantifies patient size. Finally, SSDE is the new kid on the block, but "using the effective diameter and the CTDIvol allows [it] to approximate the individual patient risk."
More people are familiar with CTDIvol and DLP right now, while fewer understand SSDE, so the idea was to find a stepwise, overlapping approach that allows for physicians' continued improvement in dose understanding and, over time, increasingly accurate reporting for authors, he said.
"We don't think that starting January 1, 2013, every author will report those as we propose," Bankier said. "It is just something that arises from our very individual experience as journal editors. But we think this is an iterative process, and every iterative process is easier to start when you go from known to unknown," and eventually become comfortable with the use of new metrics.
The proposal even applies to most retrospective studies, Bankier said. As long as the CT images are available, effective diameter can be calculated from the largest transverse and sagittal diameter of the patient. The square root of the product of those two measurements gives the effective diameter. Then, from the effective diameter and the CTDIvol of the scan, published tables (Task Group 204, American Association of Physicists in Medicine, 2011) can be used to determine SSDE, Bankier said.
The proposal isn't a rule or official recommendation; it simply represents the experience of journal editors looking for ways to provide accurate, comparable, and reproducible dose reporting methods for studies, Bankier said. And while the editors' aims are limited to clarifying reports in the radiology literature, the benefits don't stop there.
"Ultimately, I believe it does affect patient care," he said. "If you look at the speed at which dose reduction technology is implemented into new scanners, if you look at the fast pace at which these noise reduction algorithms are implemented into new scanner generations -- all based on scientific evidence -- I think this is a good example of how quickly and how directly patient care is affected by the reliability and scientific precision" of meaningful and universally understood terminology.
Owing to the importance of the issue, study drafts that arrive using imprecise terms for radiation dose won't be accepted for publication in Radiology. "We'll probably very kindly ask them to describe dose according to our recommendations -- just for our applicants," he said.