Radiation from x-ray and CT scans of the heart is low and doesn't significantly raise the risk of cancer for young children being scanned, according to a study published on June 9 in Circulation that looked at nearly 14,000 heart scans.
The authors parsed cumulative exposure data for cardiac scans given to children at Duke University Medical Center from 2005 to 2010 and computed the lifetime risk of cancer. They found an overall median effective dose of just 2.7 mSv -- lower than anticipated -- and correspondingly few deaths, even though each child received a median of 17 exams.
"Overall, for the patient cohort in the present study, cumulative effective dose was relatively low, less than the annual background exposure in the United States," the authors wrote. However, children with complex heart disease can be exposed to risks of up to 6.5% above baseline, the group noted.
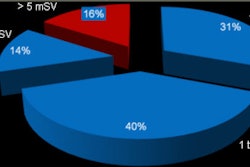
Cumulative radiation exposure
Children with heart disease are often exposed to radiation-bearing exams, which can be carcinogenic, but there are few data on cumulative exposure and the cancer risk associated with that real-life exposure, according to the authors.
"Previous studies of radiation exposure in children have largely focused on single exposure from various imaging modalities, including CT, fluoroscopy, nuclear medicine, and radiographs," they wrote (Circulation, June 9, 2014).
 Dr. Kevin Hill from Duke University.
Dr. Kevin Hill from Duke University.
But children with complex heart diseases often undergo repeat imaging. Therefore, the researchers calculated the cumulative effective dose of radiation from all exams to estimate the lifetime attributable risk (LAR) of cancer in children with heart disease over the first six years of life, senior author Dr. Kevin Hill, a pediatric cardiologist at Duke, told AuntMinnie.com.
The cohort included 337 children exposed to 13,932 radiation exams. Participants were 6 years or younger and had previously undergone one of seven primary surgical procedures: atrial septal defect closure, ventricular septal defect closure, atrioventricular canal defect repair, tetralogy of Fallot repair, arterial switch operation, cardiac transplantation, or a Norwood operation.
The study team estimated radiation dose by organ system and calculated effective dose from the sum of organ system exposures. The group estimated the cumulative risk of cancer and age- and sex-specific LAR of cancer above the baseline based on the Biological Effects of Ionizing Radiation (BEIR) VII report.
Most defects repaired were congenital, with a few procedures such as heart transplants and Norwood procedures indicating underlying heart muscle weakness -- and requiring the lion's share of radiation, said Hill. Procedures including complex heart operations and heart transplantation and a few diagnostic tests such as coronary CT angiography (CCTA) delivered higher doses than the majority of the tests, according to the authors.
Single-ventricle heart defects requiring the Norwood procedure "are probably the most complex heart defects we manage," Hill said. "Children are born with essentially half of their heart underdeveloped, and they go through a series of operations to repair the heart, and the Norwood is the first stage of that."
The overall median cumulative effective dose was 2.7 mSv (range, 0.1-76.9 mSv), with an associated LAR of 0.07% (range, 0.001%-6.5%), the study team wrote. But the median LAR varied broadly depending on the complexity of the surgery, ranging from 0.006% to 1.6% for the seven surgical cohorts. In addition, the median LAR of cancer was twice as high for females (0.04% per 1-mSv effective dose) than males (0.02%, p < 0.001).
| Exams, radiation dose, and cancer risk per surgical group | ||||
| Surgery | No. of exams per patient | Average annual dose per patient (mSv) | Cumulative dose per patient (mSv) | LAR (cancer cases per 100,000 exposed, median) |
| Atrial septal defect (n = 21) | 6 | 0.09 | 0.19 | 6 |
| Ventricular septal defect (n = 83) | 9 | 0.20 | 0.36 | 12 |
| Atrioventricular canal defect (n = 52) | 11 | 0.26 | 0.49 | 20 |
| Tetralogy of Fallot (n = 63) | 10 | 0.27 | 0.55 | 14 |
| Arterial switch operation (n = 24) | 18 | 0.29 | 0.60 | 13 |
| Cardiac transplant (n = 10) | 117 | 42.54 | 63.79 | 1,677 |
| Norwood procedure (n = 84) | 63 | 20.08 | 20.93 | 799 |
| Total (n = 337) | 17 | 1.34 | 2.67 | 65 |
Conventional invasive angiography accounted for 92% of all exams but just 8% of radiation exposure, according to the authors. Meanwhile, cardiac catheterization procedures accounted for 60% of all exposure while representing just 1.5% of exams.
High dose estimates for CCTA
Electrocardiogram-gated CCTA accounted for another 21% of all cumulative exposure and about 3% of the total exams. However, dose estimates were based on phantom studies and the technology of the era, estimating a whopping 10 mSv to 28 mSv per exam based on published estimates of the "central tendency" of the protocol, and despite the young age of participants (median age at surgery was 88 days).
"We used a combination of data to compile our dose estimates," Hill said. "Some was institutional data where we used phantoms ... with dosimeters, and we put them in the CT scanner or under the fluoroscope and quantified the dose." When that wasn't available, the authors relied on published dose estimates.
Duke was quite progressive in terms of radiation dose for the era evaluated, and "we were evaluating some of the more technologically advanced imaging protocols," he said. "But we've made further improvements since that time, and that needs to be taken into account."
Catheterization procedures, on the other hand, were calculated directly for each exam, and fluoroscopy times were all measured and entered into the dose calculator, Hill said.
The authors noted several limitations of the study, including its single-center design and the small numbers of patients for each procedure.
Lower than expected dose
The radiation dose "was lower for the average patient than we expected, but patients with more complex disease who underwent more studies sometimes had very significant long-term risk," Hill said. "Obviously everything is a risk-benefit assessment, and those patients, by virtue of having more complex disease, likely derive more benefit from having the imaging studies, but I think their lifetime risk could be substantially increased as a result of all these procedures."
In any case, the study data are consistent with epidemiological studies showing that the relative risk of cancer is highest in the early years after exposure, the authors wrote.
"For children with lower-complexity heart disease, and a presumably less complicated course, exposure was reassuringly low," they wrote. For five of seven of the procedure cohorts, the median annual effective dose of 0.09 to 0.29 mSv was substantially below background radiation levels in the U.S.
Still, aren't the risk-benefit ratios stacked heavily in favor of undergoing the exam, even considering the high 2005-era estimates of radiation dose?
"I think in nine out of 10 cases, the benefit of the study far exceeds the risk of the study, and we're certainly not advocating for not doing these procedures," Hill said. "I think the importance of these data is demonstrating to providers what the risk is so they can take steps to minimize that dose as much as possible, and also make the most informed decision regarding what types of studies they might want to perform."
It would be worth doing another study using state-of-the-art imaging techniques and today's lower doses, he said.
"I think the radiologists have done a great job [in dose reduction], and the cardiologists are behind the radiologists in terms of technological advances," Hill said. "We're catching up, but I think the cath protocols are where some of the greatest benefits can be derived in the next several years."