CHICAGO - Radiologists from the Bronx who took a rare look at a typically underserved poor community found substantially more lung cancers than have been seen in other studies, including the National Lung Screening Trial (NLST).
The ongoing study at Montefiore Medical Center has evaluated, to date, some 320 asymptomatic individuals. The researchers found that more than 2.5% of the poorer and more overweight population had lung cancer, compared with approximately 1.5% in most screening trials serving a larger mix of more affluent and predominantly white subjects.
The inner city population also had advanced disease, however, calling into question the utility of screening for lung cancer using NLST criteria.
 Dr. Hanna Milch from Montefiore Medical Center.
Dr. Hanna Milch from Montefiore Medical Center."Our Bronx population was different from that of the National Lung Screening Trial," said Dr. Hanna Milch from Montefiore Medical Center. "Only one patient had stage I disease, so it's unclear whether the mortality benefits found in NLST are generalizable to our Bronx population."
The state of New York this year awarded the Bronx the dubious distinction of unhealthiest county, and it's not hard to see the reasoning behind it. Eighty percent of the population is covered only by Medicare or Medicaid. Most screening subjects were overweight, with an average body mass index of 31, and most still smoked. More than two-thirds were nonwhite, with a large proportion of immigrants.
"The goal of our screening program is to save lives," Milch said. "To do this, we need to determine if the mortality benefits found in NLST are generalizable to the predominantly poor, inner city, overweight population of the Bronx."
Dr. Alla Godelman, Milch, and colleagues screened the first subject for lung cancer in December 2012. Based on NLST criteria, subjects were required to have a minimum 30 pack-year smoking history and be asymptomatic at the time of screening. They were also required to have a physician referral and pay a discounted $25 fee for screening if they did not have insurance coverage.
Key to the program is a bilingual screening coordinator who schedules, tracks, and follows up all patients with the help of a specially tailored screening component added to the electronic medical record (EMR), Milch said. The patient coordinator also serves as a liaison between patients, radiologists, and the referring physician.
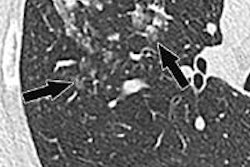
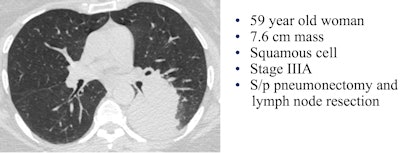 Image courtesy of Dr. Hanna Milch.
Image courtesy of Dr. Hanna Milch.To assess risk, the group created a standardized "Bronx score" that estimates lung cancer probability similar to the BI-RADS model for breast cancer. A Bronx score of 1 or 2 means the CT was negative or there were benign findings, resulting in a follow-up screen in one year. A score of 3 or 4 means that detected nodules or opacities require a shorter-term follow-up, and a score of 5 means a high suspicion of malignancy. Radiation dose was recorded for each scan.
In all, 320 of the referred patients were screened for lung cancer, and nine had a score of 5 on the Bronx score, eight of whom went on to receive a histology-proven lung cancer diagnosis. The ninth patient's CT scan was highly suspicious for malignancy, but the patient has not yet had a tissue confirmation.
Compared with the NLST population, the Bronx patients were older (64 versus 60 years), more were current smokers (68% versus 48%), and chronic diseases were much more prevalent, Milch said. For example, 34% (compared with 17% for NLST) had chronic lung disease, 60% (versus 35%) had hypertension, and 38% (versus 28%) were obese. As for demographics, only 26% of the Bronx screening subjects were white, compared with 91% in the NLST population.
Of the eight patients with confirmed lung cancer, just two had adenocarcinomas, which are more often curable, and only one patient had stage I disease.
| Bronx vs. other lung cancer screening trials | |||
| Study | Prevalence | Stage I | Adenocarcinoma |
| Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) | 0.9 | -- | -- |
| NLST | 1.1 | 54% | 56% |
| International Early Lung and Cardiac Action Program (I-ELCAP) | 1.3 | 85% | 76% |
| Mayo Clinic | 1.3 | 70% | 70% |
| Bronx | 2.5 | 13% | 25% |
In other lung cancer screening trials, adenocarcinomas were the dominant cancer type, but this was not the case in the Bronx trial, Milch said. Even so, the Bronx trial's reported prevalence of 2.5% may reach as high as 2.8% if the ninth patient is confirmed to have lung cancer.
As for limitations, the population tends to be under financial strain, making lung cancer screening a low priority for many eligible individuals, she said. Moreover, the high prevalence of obesity affects image quality as well as the radiation dose.
The fact that only one patient had stage I disease "makes it unclear if the mortality benefits found in the NLST population are generalizable to our Bronx population," Milch said.
In any case, screening continues, and further results may answer some of the important questions surrounding lung cancer screening in this population, she told AuntMinnie.com.