New research with CT supports the hypothesis that lung adenocarcinoma may spread through the airways and not just through the blood. So-called aerogenous metastasis of lung cancer has implications for staging, management, and prognosis and may be underrecognized, the authors report in the American Journal of Roentgenology.
In fact, growing evidence suggests that aerogenous metastasis may be more common than hematologic spread. Imaging features on CT also could help determine when aerogenous spread may be occurring (AJR, December 2014, Vol. 203:6, pp. W570-W582).
Blood vs. airway spread
Lung cancer, the most common cause of cancer death worldwide, has a five-year survival rate of 6% to 18%, the authors wrote. Adenocarcinoma accounts for as many as 30% of cancer cases.
The article, by Dr. Anand Gaikwad and colleagues from the University of Ottawa in Canada, aims to summarize relevant literature on aerogenous metastasis, and explain the likely pathogenic mechanism of aerogenous spread, showing characteristic imaging and pathologic features.
Local venous spread can occur via pulmonary venous invasion and proximal venous metastasis within the lung, but systemic spread is much more common, the authors wrote. Cancer cells pass through common sites of metastatic disease, such as the liver, adrenal glands, bones, and cerebrospinal fluid, before they return to the heart and pulmonary arterial circulation, and ultimately back to the lungs, they explained.
At CT, lesions of such lung metastases spread via the circulatory system are characteristically distributed randomly; round nodules are easily recognizable at CT and pathologic examination. On the other hand, aerogenous metastasis is defined as discontinuous spread of cancer cells from the primary tumor through the airways to adjacent or distant lung parenchyma.
CT features
CT features that strongly suggest aerogenous spread include "persistent centrilobular nodules and branching opacities (tree-in-bud nodules), typically with ill-defined margins and ground-glass attenuation," the study team wrote. Well-defined nodules with soft-tissue attenuation are less common in this scenario.
Nodules suggestive of aerogenous spread tend to be clustered, and they always show evidence of growth on serial images, they wrote. In some cases, they progress to confluent air-space disease.
When these metastases are remote from the primary lesion, the nodules tend to have a dependent distribution in the lower lobes. The appearance on CT "reflects cancer cells lining the small airways and alveolar spaces in a lepidic pattern with variable amounts of intra-alveolar material," the authors explained.
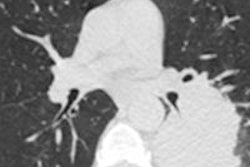
 CT features of aerogenous spread of tumor. Image shows primary lung adenocarcinoma in right middle lobe presenting as air-space consolidation in 49-year-old female nonsmoker. Centrilobular nodules (arrow) and acinar opacities are present away from primary lesion in different bronchial territory. Images republished with permission of the American Roentgen Ray Society.
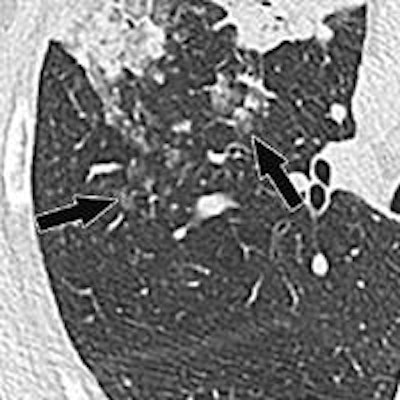
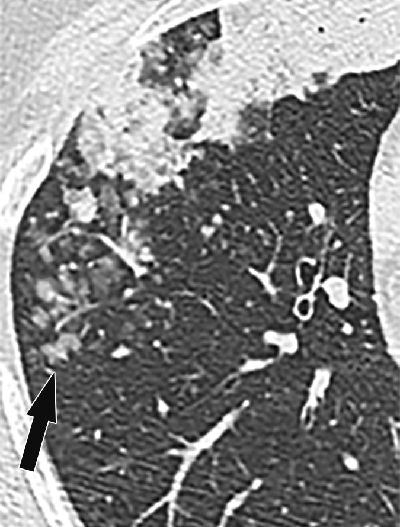
CT features of aerogenous spread of tumor. Image shows primary lung adenocarcinoma in right middle lobe presenting as air-space consolidation in 49-year-old female nonsmoker. Centrilobular nodules (arrow) and acinar opacities are present away from primary lesion in different bronchial territory. Images republished with permission of the American Roentgen Ray Society. CT image shows primary lung invasive mucinous adenocarcinoma in right upper lobe presenting as air-space consolidation with air bronchograms in 68-year-old man. Ill-defined centrilobular nodules (arrows) with ground-glass attenuation are present posterior to lesion.
CT image shows primary lung invasive mucinous adenocarcinoma in right upper lobe presenting as air-space consolidation with air bronchograms in 68-year-old man. Ill-defined centrilobular nodules (arrows) with ground-glass attenuation are present posterior to lesion."Growing evidence in the literature suggests that aerogenous spread of lung adenocarcinoma is an underrecognized form of tumor progression, having distinct pathologic and imaging findings and potentially major management implications," the authors concluded. "The presence of persistent or growing centrilobular nodules on CT images should be considered suspicious for aerogenous spread in patients with primary lung adenocarcinoma, particularly those with invasive mucinous, papillary, and micropapillary subtypes."
Aerogenous metastases must be differentiated from multiple synchronous lesions in the spectrum of lung adenocarcinoma, they wrote. Appropriate diagnosis and treatment requires a multidisciplinary approach that includes radiologists, thoracic surgeons, pathologists, and geneticists. Genetic profiling can help provide proof of monoclonality in cases where aerogenous metastasis is suspected.