Nearly half of patients who receive radiologist recommendations for chest CT to evaluate abnormal findings on chest radiography have clinically relevant findings at CT, including a substantial number of new malignancies, according to a new study in Radiology.
Of nearly 30,000 chest radiographs performed at Massachusetts General Hospital (MGH) in 2008, about 4.5% were referred for CT owing to something suspicious seen on the radiograph. Among the chest x-rays that were actually followed up, the researchers found a rate of abnormalities on chest CT greater than 40%, and of these, more than 8% harbored a previously unknown cancer, the authors reported (Radiology, December 22, 2014).
"A very high proportion of those [referred] cases led to something that was clinically significant -- either an important new diagnosis or something that would require further workup," said MGH radiologist and co-author Dr. Tarik Alkasab, PhD, in an interview with AuntMinnie.com.
Requests for additional imaging (RAIs), especially CT, have soared in the past decade, up as much as 200% since 1995. The growth has generated loud questions about the potential of overreferral, and suggestions that radiologists may be responsible for part of an unnecessary increase in imaging rates.
Too much CT?
"People have talked about increasing imaging rates and that has raised concerns about whether it's driving up the cost of imaging or creating inconvenience for patients, but no one had yet tried to determine what the value of that additional imaging was," Alkasab said. "We said it's hard to talk about whether it's a good thing until we know what it leads to."
 Dr. Tarik Alkasab, PhD, from Massachusetts General Hospital and Harvard School of Medicine.
Dr. Tarik Alkasab, PhD, from Massachusetts General Hospital and Harvard School of Medicine.The study authors looked at a specific clinical situation, in which a radiologist is examining a chest x-ray and decides something is questionable and decides the patient should have a CT scan to see what the questionable finding is, Alkasab said.
Enrollment was limited to outpatients 18 years and older who hadn't had a CT scan in the past five years. The group further looked at who had been referred for a CT scan and how many of those patients actually had the CT -- which was about 70% or 705 individuals.
In all, some 4.5% (1,316) of the 29,138 outpatient radiography exams contained a recommendation for chest CT, and the probability of a referral was related to increasing patient age (p < 0.001) and positive smoking history (p = 0001).
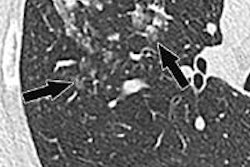
Chest CT scans were performed on 16- and 64-detector-row scanners from GE Healthcare and Siemens Healthcare. The images were reviewed by board-certified radiologists, and the group further looked at the finding in relation to the reason for the recommendation.
"So if the radiologist was talking about something on the upper lobe of the right lung, we made sure that if we were seeing something on CT it was what the radiologist was referring to," Alkasab said.
CT recommendation rates for each of the 11 interpreting thoracic radiologists ranged from 2.5% to 8.7% (mean, 4.7%), and there was an insignificant trend toward lower follow-up recommendation rates among thoracic radiologists with more years of experience, the group wrote.
Among the 65.4% of patients who actually went through with the follow-up CT, the study team detected clinically relevant findings that corresponded to the reason for the referral in 41.4% (286 of 691) studies, the study authors wrote.
Insignificant findings at CT were seen in an additional 20% of cases, and about 38% contained no corresponding abnormalities. At the same time, newly diagnosed, biopsy-proven malignancies were found in 8.1% (56 of 691) cases that underwent follow-up CT.
"What was really shocking was the number that turned out to be new malignances -- it was a pretty significant percentage," he said.
Mainly lung cancers
In all, 41 of the 56 biopsy-proven malignancies were lung cancer (including 27 adenocarcinoma, five squamous cell carcinomas, two non-small cell carcinomas, and six small cell carcinomas), Alkasab said. There were 12 lung metastases, three mediastinal lymphomas, and two Hodgkin's lymphomas in the mix as well.
A radiologist's recommendation for chest CT to examine an abnormal chest radiography finding provides a high yield of clinically relevant findings, the study team concluded.
"Because the U.S. healthcare system is shifting from volume-driven to value-based payment models, it is increasingly important for the radiology community to validate the clinical effect of abnormalities and a lower threshold for radiologists to recommend a chest CT examination in these patients," wrote Alkasab, along with lead investigator Dr. H. Benjamin Harvey, Dr. Matthew Gilman, Dr. Carol Wu, and colleagues.
Study limitations included its performance at a single academic medical center with a large percentage of specialists referring cases, which might limit the generalizability of the results to nonreferral centers or private practices, the group wrote. Also, the study did not capture the results of follow-up imaging performed at outside institutions.
"To me, the big point of our study is that a lot of recent focus on radiologist recommendations is how do we decrease recommendations -- and what this study points out is that maybe it's possible to actually be recommending too little," Alkasab said.
What needs to be done is to figure out the right level of recommendation for specific clinical situations, then help radiologists get to that level, he noted.
"I don't know specifically what the right level of recommendation is for this situation, but it's possible that we're recommending too few CTs based on these x-rays," Alkasab said. "A positive predictive value of finding something significant of 40% means that maybe we're not recommending enough of them."
Once you get to that level and you know the yield of a follow-up exam, you can start to put together an entire cost-benefit model, he said, weighing all the negatives of a follow-up exam, such as cost, possibility of overdiagnosis, or excess malignancy, against all the positives, such as getting an earlier and more timely diagnosis, he said.
"That's the kind of process that has to go into the question of what is the right recommendation rate, and this can help radiologists guide their practice," Alkasab said.
The group is going forward on a couple of fronts, including seeing if there is anything radiologists can do to increase the rate at which follow-up exams are actually obtained, since as many as one-third of these recommendations may not have been followed up on, he said. What factors affect compliance? Does the wording of the radiology report play a role?
"The other piece we'd like to move forward on is putting into place systems that have structured recommendations that contain all the information that downstream systems would need for the referring physicians to order that follow-up test, and taking down barriers that affect compliance," he said.