
When it comes to arterial plaque, researchers are beginning to believe that soft, noncalcified plaques rather than arterial calcifications are the real killers. In a study published online June 2 in Radiology, U.S. National Institutes of Health (NIH) researchers used CT to measure soft plaques and tie their size to risk factors for heart disease.
Senior author Dr. David Bluemke, PhD, along with colleagues from NIH and also Johns Hopkins University, found that CT-based measurements of noncalcified plaque matched up well with other known risk factors for cardiac disease, such as elevated low-density lipoprotein (LDL) cholesterol levels, systolic blood pressure, and diabetes. The group developed a quantitative index for assessing both soft and total plaque burden that approximates intravascular ultrasound, currently the gold standard for imaging plaque burden.
The new index could be a better method for determining cardiac risk than using CT-generated calcium scores alone. It could also be an improvement over intravascular ultrasound, which can measure noncalcified plaque but, due to its invasive nature, is not well-suited for asymptomatic individuals.
CT measurements of coronary artery calcium (CAC) such as Agatston scores have become an accepted tool for measuring calcified plaque burden and have been connected to a higher risk of heart disease. But CAC scores do not measure noncalcified plaque, also known as atheromas, which some believe could be even more dangerous than calcified plaque because they are more prone to rupture and cause a cardiac event.
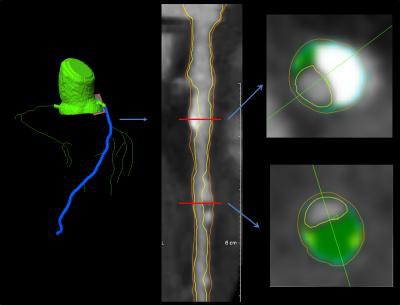 Images from a 62-year-old man. Left: coronary segmentation model of the coronary tree. Middle: curved multiplanar reconstruction of the left anterior descending artery, with the lumen and external vessel walls marked. Right: representative cross-sectional images, with green shading as noncalcified plaque. Images courtesy of RSNA.
Images from a 62-year-old man. Left: coronary segmentation model of the coronary tree. Middle: curved multiplanar reconstruction of the left anterior descending artery, with the lumen and external vessel walls marked. Right: representative cross-sectional images, with green shading as noncalcified plaque. Images courtesy of RSNA.The researchers hypothesized that risk factors for the presence of noncalcified plaque could differ from those for calcified plaque, so they set out to compare associations between the factors and measurements of these different types of arterial plaque.
The group began with a population of 202 men and women (64% men; mean age, 65.5 years) who were eligible for statin therapy and who had been evaluated as part of a baseline assessment in the Randomized Trial of Imaging Versus Risk Factor-Based Therapy for Plaque Regression (Radiology, June 2, 2015).
The participants received a battery of tests to calculate risk factors and then underwent CT scanning with a 320-detector-row scanner (Aquilion One, Toshiba America Medical Systems). Plaque analysis was performed with commercially available workstation software (QAngio CT version 2.0, Medis Medical Imaging Systems).
The researchers used the software to calculate total plaque volume, which consisted of both calcified and noncalcified plaque volume, and then plaque burden per unit length, which consisted of segmental plaque volume in cubic millimeters, divided by the length of the arterial segment in millimeters. This yielded a total plaque index in square millimeters; the noncalcified plaque index was calculated by subtracting the volume of calcified plaque from the total volume.
After adjusting for age, gender, and the use of statins, the noncalcified plaque index showed a statistically significant correlation with three risk factors: systolic blood pressure (p < 0.03), LDL cholesterol level (p < 0.02), and a diagnosis of diabetes (p < 0.03), the researchers found. This compares to correlation with only two risk factors (male gender and statin dose level) for the total plaque index and one risk factor (male gender) for Agatston CAC score.
The findings indicate that the noncalcified plaque index could be a better barometer than total plaque index or Agatston CAC scores, the group concluded. The results are especially significant given related research that suggests statin therapy has a major effect on noncalcified plaque volume, even as calcified plaque volume remains unchanged.
"The message is that in these low- to moderate-risk individuals, it was uniquely the noncalcified plaque index that related most closely to important risk factors such as LDL and blood pressure," Bluemke wrote in an email to AuntMinnie.com. "The CAC contributes heavily to the overall total plaque index: Both of these were not very revealing."




















