
A new technique that calculates fetal dose from CT scans given to pregnant women is accurate and easy to perform, according to a study presented at this week's American Association of Physicists in Medicine (AAPM) 2015 annual meeting in Anaheim, CA.
The method, which factors in the size of the patient expressed as a water-equivalent diameter, can be used on any CT scanner, concluded researchers from the David Geffen School of Medicine at the University of California, Los Angeles (UCLA).
"A reasonably accurate dose to the fetus can be obtained by knowing simply the scanner output and the size of the patient expressed in the water-equivalent diameter," said lead author Michael McNitt-Gray, PhD, a medical physicist and professor in the department of radiology at UCLA, in a July 15 teleconference.
Can we scan the patient?
The need to scan a pregnant patient, such as to check for bleeding after a car accident or for blood clots given signs of pulmonary embolism, always raises concerns about the risks of radiation to the fetus.
Patients and clinicians who need the scans aren't always sure if a pregnant woman can safely be scanned. Even more commonly, a pregnant woman will undergo a clinically indicated CT scan before she even knows she is pregnant, McNitt-Gray said.
"The purpose of this study was to provide tools to easily and accurately estimate the radiation dose to the fetus," he said.
The research team developed patient size-specific, scanner-independent conversion coefficients for CT dose index volume (CTDIvol) to fetal dose. The coefficients were developed for abdominal and pelvic CT exams of pregnant patients who had a gestational age ranging from 12 to 36 weeks.
"Those are the scans that go right through the region where the fetus would be," McNitt-Gray said.
The study advances earlier techniques for estimating radiation dose by accounting for patient size and composition using water-equivalent diameter. The method enables better characterization of patient size than simple measurements and, as a result, provides more accurate estimates of the radiation dose to the fetus.
"The information we provide usually is not only comforting to the patient, it's comforting to the physician who is trying to comfort the patient," McNitt-Gray said in a statement.
The research team created models of fetal anatomy from image data from 18 pregnant women who had undergone abdominal/pelvic CT. They estimated fetal doses for each model using Monte Carlo simulations of fixed tube current CT scans with 64-detector-row scanners from Philips Healthcare, Toshiba Medical Systems, Siemens Healthcare, and GE Healthcare.
Scanner-independent CTDIvol-to-fetal-dose conversion coefficients for each fetal dose patient were created by normalizing scanner-specific 32-cm CTDIvol values across all four scanners.
Patient sizes were depicted using water-equivalent diameter measurements taken from the image containing the 3D geometric centroid of the fetus.
The researchers then calculated the coefficient of variation across the four scanners for the simulated fetal dose before and after CTDIvol normalization to show the utility of CTDIvol-to-fetal-dose conversion coefficients for each patient, according to the study abstract.
Dose correlated with 2 measures
"We found a nice relationship between radiation dose to the fetus and a couple of other reasonably available values, such as the radiation dose output metric or CTDIvol, a value that's already reported on the CT scanner console ... and the water-equivalent diameter," McNitt-Gray said.
The coefficient of variation across the scanners for fetal dose in all patients ranged from 25.10% to 30.16% before CTDIvol normalization to 5.60% to 9.48% after normalization.
The researchers also found an exponential relationship between CTDIvol-to-fetal-dose conversion coefficients and patient size, with a coefficient of determination of 0.84.
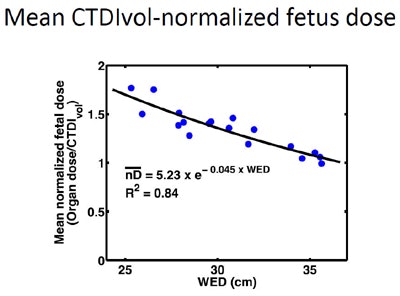 Graph shows that estimated fetal doses using water-equivalent diameter (WED) and CTDIvol (blue dots) correlate well with measured fetal doses (black line). Estimated fetal doses declined as patient size increased. Image courtesy of Michael McNitt-Gray, PhD, and co-authors, UCLA.
Graph shows that estimated fetal doses using water-equivalent diameter (WED) and CTDIvol (blue dots) correlate well with measured fetal doses (black line). Estimated fetal doses declined as patient size increased. Image courtesy of Michael McNitt-Gray, PhD, and co-authors, UCLA.There is a strong correlation between CTDIvol normalized fetal dose and water-equivalent diameter, the group concluded. The results show that fetal dose from abdominal and pelvic CT examinations of pregnant patients of various gestational ages can be accurately estimated using just two factors:
- Fetal dose normalized by CTDIvol to account for scanner variation
- Water-equivalent diameter patient-size metric to account for size variation
"We hope it's a very helpful and useful tool for the medical physicist in a very difficult situation," McNitt-Gray said.
The researchers are gathering new data for a similar study that uses automatic exposure control (AEC) rather than fixed tube currents, as AEC is more common now, McNitt-Gray said in response to a question from the audience.




















