As demand for imaging and the use of CT in the emergency department grow, the probability of both planned exposures in pregnancy and inadvertent exposures also is increasing. Is it likely that both scenarios will be encountered by most imaging departments several times a year, so radiologists must be prepared for this eventuality, delegates will hear at today's Special Focus Session on CT in pregnant patients and the dilemma it poses for the radiologist and the mother.
To explain options and facilitate justification, as required by European Union Council Directive 2013/59 on radiation protection, open disclosure and good multidisciplinary teamwork are crucial components of communication, according to Paddy Gilligan, chief physicist at Mater Private Hospital in Dublin, who will be speaking about dose risk and communication to referring physicians and patients.
Recent experiences in Ireland of trying to develop practical guidance for radiation safety and how to address pre-exam pregnancy status showed that expert consensus was difficult to achieve. Furthermore, different working practices, such as imaging at centers where no radiologist is available, highlight the need for an existing communication plan about who will speak to the patient and what will be said.
"Be 'fetal exposure fit.' Experience has shown that the majority of fetal exposures take place with minimal warning," he told ECR Today ahead of the congress. "Make sure that you have accurate information and involve the patients in their care and that your messages are clear. When good practices are in place alongside improved dosimetry and optimization techniques, the risks are small."
Effective communication also is based on trust, and this can only be fostered through comprehensible, consistent, and accurate information delivered in a stress-free environment, he noted.
"Patients are reassured when good radiation protection culture is evident. The literature has shown that increasing proactive radiation risk information available on both social media and traditional media helps when such information is required as part of decision-making," Gilligan said.
However, Irish research has revealed the use referrers make of web-based referral guidelines containing risk information was much lower than anticipated. Although the number of hits from Irish users on the Royal College of Radiologists' Irefer Website rose from 493 in 2013 to 763 in 2015, absolute numbers suggest measures need to be taken to promote greater use of the adopted guidelines, he continued.
Many national bodies require inadvertent fetal exposures to be reported. In 2016, there were five such exposures in Ireland -- three in radiotherapy and two in radiology -- out of 2 million radiological procedures, highlighting low national incidence.
There are many reasons why a pregnancy might be overlooked, according to Gilligan. For instance, a patient who is placed on a CT waiting list in March and who turns up in October in the early stages of pregnancy for the exam may not be picked up by routine questioning or by pregnancy testing. The same can be true in cases where urgent PET/CT scans don't follow usual scheduling. In both scenarios, the booking and processes used, and education of radiology staff, referrers, and patients will play a central role, and it did in follow-up actions recommended after the five 2016 exposure incidents, he noted.
Radiologists and referrers need to raise their game when it comes to knowledge related to patient doses and associated risks, and particularly risks to the fetus, according to John Damilakis, PhD, director of the department of physics at the University Hospital of Iraklion in Crete.
"Surveys show that there is lack of knowledge of conceptus dosimetry in the imaging of pregnant patients. This may lead to poor patient care and inappropriate advice," he said.
Damilakis' presentation on "conceptus dosimetry methods" will provide information about how to manage pregnant patients properly from the point of view of radiation protection and an overview of the dosimetry methods and tools available.
"Conceptus dose evaluation is needed whenever pregnant patients are exposed to x-rays. Specific measurements and detailed calculations of conceptus doses are necessary if these doses are suspected of exceeding 10 mGy," he said.
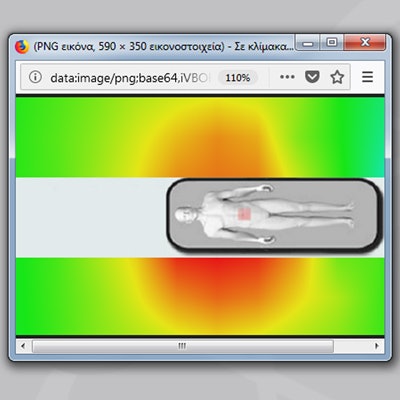
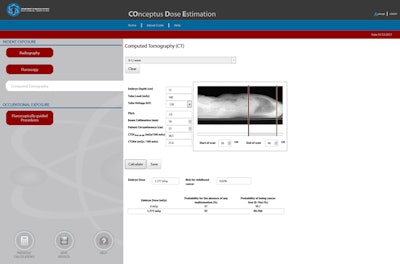
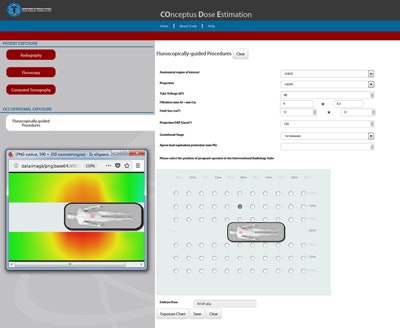
He will provide the latest information about conceptus dose estimation tool, CoDE, a free web-based software tool developed by the University of Crete School of Medicine. The dynamic tool establishes conceptus dose and risk assessment from x-ray imaging examinations and calculates fetal dose in cases of occupational exposure. The software also can be useful for education and training, as well as developing dose reduction strategies, said Damilakis, adding that around 500 European health professionals have subscribed to CoDE.
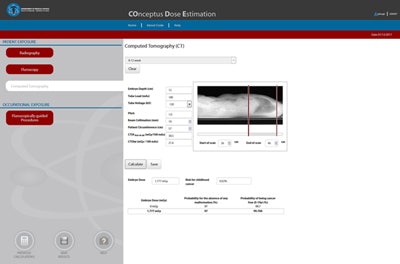
These figures show CoDE screens for entry of scan parameters for the estimation of conceptus dose and risk. Images courtesy of John Damilakis, PhD.
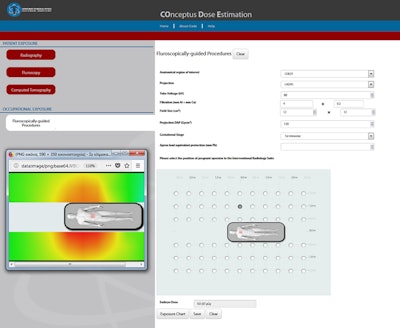
These figures show CoDE screens for entry of scan parameters for the estimation of conceptus dose and risk. Images courtesy of John Damilakis, PhD.
Such methods are vital for estimating radiogenic risk during any justification and optimization process for CT examinations in pregnant patients. For example, if a pregnant patient with abdominal pain was admitted to a hospital to rule out appendicitis, but the appendix was not visualized adequately with ultrasound, physicians might request abdominal CT with and without contrast. "Radiologists need to weigh up the risk of irradiating the conceptus against that of not making the necessary diagnosis," he said.
Dose estimation tools can also help the relevant parties take important decisions in cases of accidental exposure during the first postconception weeks. For instance, if a woman undergoes an interventional procedure in the abdominal area and then finds out after the procedure that she was six weeks pregnant, should her obstetrician recommend abortion?
"Conceptus doses below 100 mGy should not be considered a reason for abortion," he concluded. "Dose estimation tools provide information useful for the dose and risk management of pregnant patients. However, it is important to mention that dose and risk values provided by such tools should be taken as estimates and can be used for general guidance only."
Originally published in ECR Today on 1 March 2018.
Copyright © 2018 European Society of Radiology