In today's Special Focus Session, experts will provide an update on imaging modalities, treatment strategies, and therapy monitoring in patients with musculoskeletal (MSK) tumors, aiming to raise awareness of how multimodality imaging can influence therapeutic balancing between tumor control and quality of life.
Musculoskeletal tumors are a rare and diverse group; therefore, a wide range of tumors and tumor-like conditions may be encountered when patients undergo radiological examinations. Because of the advent of new chemotherapeutic drugs and treatment regimens, and, as a result of advances in imaging and surgical techniques, the prognosis of patients with musculoskeletal tumors has improved over the last years, as Dr. Johan Bloem, PhD, from the department of radiology at the Leiden University Medical Center in the Netherlands and chair of this session, will illustrate.
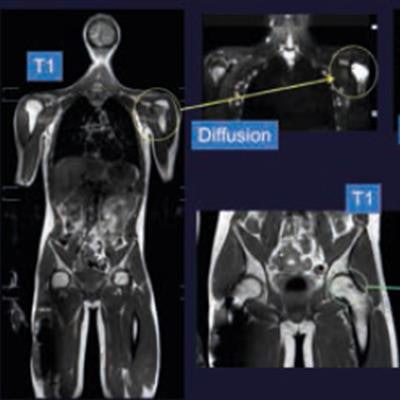
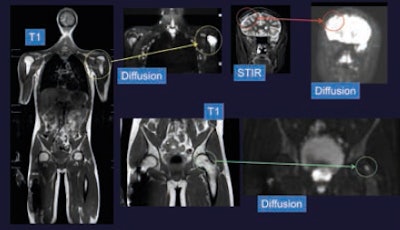 Ewing sarcoma, previous resections of the right femur and lumbar spine. Ewing metastases on this whole-body MRI are visible on T1-weighted and diffusion images in the left humerus, left femur, and right cranial vault. Images courtesy of Dr. Johan Bloem, PhD.
Ewing sarcoma, previous resections of the right femur and lumbar spine. Ewing metastases on this whole-body MRI are visible on T1-weighted and diffusion images in the left humerus, left femur, and right cranial vault. Images courtesy of Dr. Johan Bloem, PhD."Diagnostic tests in combination with systemic and focal therapy are used to reach curative or palliative goals. The progress made in diagnostic tests, treatment strategies, and understanding the biologic behavior of tumors increases our options to serve our patients," he emphasized.
However, there is also another side to the coin, as these developments increase therapy-related morbidity, diagnostic test-related anxiety, follow-up invasive procedures, and costs.
"The current challenge is to use our diagnostic and therapeutic means to increase not only survival chances but to also preserve quality of remaining life, while involving the patient's opinion into decision-making processes," Bloem noted.
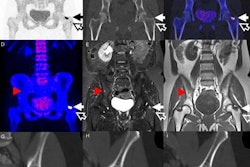
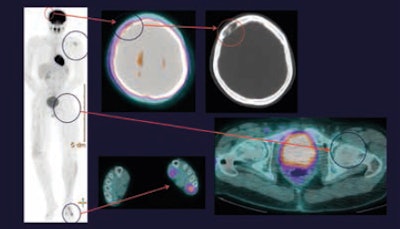 On PET/CT, the metastasis in the left humerus is FDG-positive, but the metastasis in the right cranial vault is FDG-negative and only seen on the corresponding CT scan. The metastasis in the left femur is invisible on the PET/CT scan. Note increased FDG uptake in left leg and foot secondary to muscle activity.
On PET/CT, the metastasis in the left humerus is FDG-positive, but the metastasis in the right cranial vault is FDG-negative and only seen on the corresponding CT scan. The metastasis in the left femur is invisible on the PET/CT scan. Note increased FDG uptake in left leg and foot secondary to muscle activity.As medical treatment is becoming more individualized due to a better understanding of tumor pathophysiology in relation to various available treatment options, in the future, the aim is to better tailor treatment goals to the patient's needs. Imaging plays a key role in establishing the diagnosis, determining prognosis, selecting treatment strategies, monitoring the treatment effect, and detecting recurrence.
"However, until now only medical judgment, which is based on imaging, has been used to set therapeutic goals, while a patient's needs and lifestyle were hardly taken into account. Now, potential benefits to the patient in relation to potential difficulties, which arise in the course of the disease, such as comorbidities of treatment, complications, and loss of function, as well as individual needs are becoming increasingly important. This is essential, as, for example, a 19-year-old male who spends most of the time in front of a PC has completely different needs to a 50-year-old marathon runner," Bloem explained.
"Age has always been an important parameter when evaluating musculoskeletal tumors; however, against the background of an aging population and major differences in regard to lifestyles, it is no longer sufficient," he added.
Bloem plans to specifically outline the demand for new treatment concepts. "The combination of morphological and especially functional imaging with MR and PET/CT provides detailed information on the phenotype of the tumor. Thus, it is possible to better predict how the tumor will behave and respond to treatment. Combining this information with patient characteristics allows us to make treatment decisions together with the patient and to balance advantages and disadvantages of different treatment strategies," he said.
The impact of treatment choices on survival chances and quality of life will also be a central theme of the presentation of Dr. Michiel van de Sande, from the department of orthopedic surgery at the Leiden University Medical Center, who, among other things, plans to discuss options that allow providing better individualized treatment strategies and strategies for personalized postsurgical follow-up.
"Knowing if the sarcoma will return remains the basic patient paradigm in cancer treatment and follow-up. All currently available prediction models for sarcoma are applicable only at the time of baseline, such as at the time of diagnosis or surgery. Updated patient information during the follow-up and changing covariate effects over time may change the prognosis. However, this is not taken into account in currently available models," van de Sande explained.
The concept of dynamic prediction allows the inclusion of updated information on the status of the disease, patient characteristics, and imaging results during the follow-up, which can be used to provide better individualized treatment and follow-up options depending on the dynamic assessment of a patient's prognosis.
During this session, van de Sande plans to familiarize ECR delegates with a multicenter analysis and the dynamically predictive Personalized Sarcoma Care model (PERSARC), which supports shared decision-making in high-grade extremity soft-tissue sarcomas (STS). The model considers treatment modalities, including applied radiotherapy and achieved surgical margins, and predicts overall survival as well as the probability of local recurrence (LR) at three, five, and 10 years.
To this end, an app was developed to assist in shared decision making in clinical practice.
"During the follow-up, we analyzed the timing of LR and distant metastasis (DM), concluding that in patients with localized STS after curative surgery, rates of LR and DM are highly nonconstant over time and strongly modified by tumor characteristics. These findings contradict a 'one-size-fits-all' aftercare policy and support the concept of a time and risk-adapted strategy for personalized post-surgical follow-up," he explained.
At present, patients are mainly being advised based on local experience but not always on evidence. Allowing individualized treatment plans, this app might change that, according to van de Sande.
"Radiology will help to further enhance the model in regard to tumor location, size, and, in the future due to PET and dynamic MRI, also biological behavior. Also, follow-up scans will be added to the model, helping to individualize the follow-up protocol in order to minimize hospital visits and anxiety and to maximize the screening yield," he concluded.
Bloem and van de Sande will be joined by Dr. Marc-André Weber, from the University Medical Centre Rostock in Germany, and Dr. Christina Messiou, from the Royal Marsden National Health Service Trust in London, who will discuss multimodality imaging in the treatment of bone and soft-tissue sarcoma.
Originally published in ECR Today on 4 March 2018.
Copyright © 2018 European Society of Radiology