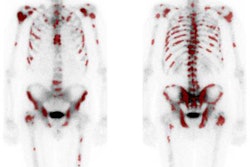
Despite the apparent technological advantages of SPECT/CT, PET/CT, and PET/MRI, the three hybrid modalities do not perform appreciably better than planar bone scintigraphy in detecting and diagnosing bone metastases, according to a study published online August 10 in the Journal of Nuclear Medicine.
Researchers in Denmark conducted a head-to-head comparison of all four modalities and found no statistically significant difference in sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), or overall accuracy when equivocal readings were excluded.
"[Sodium fluoride (NaF)] PET/CT and whole-body SPECT/CT resulted in a significant reduction of equivocal readings compared to planar bone scintigraphy, which implies an improved diagnostic confidence," wrote lead author Dr. Johan Löfgren and colleagues from the University of Copenhagen. "However, the clinical benefit of using [NaF-PET/CT] or PET/MRI as compared to SPECT/CT and planar bone scintigraphy in this patient population with a relatively low prevalence of bone metastases (14%) is likely limited" (JNM, August 10, 2017).
Modalities of choice
Contrast-enhanced planar bone scintigraphy with technetium-99m (Tc-99m)-labeled radiopharmaceuticals, such as hydroxyethylene diphosphonate (Tc-99m HDP), remains the most frequently used method for diagnosing bone metastases. However, previous research has shown that adding SPECT/CT to planar bone scintigraphy can improve specificity, PPV, and diagnostic confidence, thus reducing the number of equivocal reports.
There are also advocates for NaF-PET/CT imaging for bone metastases, given the hybrid modality's efficacy in oncologic applications and shorter uptake time from NaF administration to scanning, compared with planar bone scintigraphy. Whole-body MRI has also gained attention, with its ability to detect early bone marrow lesions compared to CT, and combining it with NaF-PET could further improve bone metastases evaluation.
Löfgren and colleagues therefore decided to compare planar scintigraphy with three combinations: SPECT/CT, PET/CT, and PET/MRI. They prospectively enrolled 117 patients between June 2012 and January 2015 who were referred for clinical planar bone scintigraphy and met the study criteria. The cohort included 62 men with prostate cancer, 54 women with breast cancer, and one woman with renal cancer.
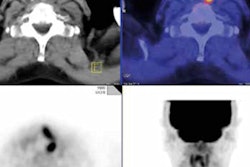
Standard planar bone scintigraphy and whole-body SPECT/CT scans were acquired in one session using a hybrid SPECT/CT scanner (Symbia, Siemens Healthineers, or Precedence, Philips Healthcare) featuring a dual-head, variable-angle gamma camera with a 16-slice helical CT scanner. Patients were imaged for approximately 25 minutes in the supine position three hours after injection of Tc-99m HDP (586 ± 27 MBq; range, 523-655 MBq).
Whole-body NaF-PET/CT imaging (Biograph mCT or Biograph TrueV, Siemens) was performed 5.3 (± 2.3) days after planar bone scintigraphy and SPECT/CT in the supine position, approximately 45 minutes after injection of sodium fluoride (210 ± 13 MBq; range, 151-239 MBq). Scan time was approximately 30 to 35 minutes.
Finally, simultaneous NaF-PET/MRI (Biograph mMR, Siemens) was performed on 46 patients with a head/neck coil and four body surface coils after the NaF-PET/CT scan. Mean time from injection to scan was 124 (± 23) minutes (range, 89-181 minutes).
The researchers used histologically confirmed diagnoses, clinical follow-up of at least six months, biopsies, or other imaging studies for the reference standard. The average follow-up period was 652 (± 217) days (range, 130-1,090 days).
Each scan was categorized on a per-patient basis as benign (no bone metastases), equivocal, having bone metastases present, or having widespread metastases (> 20 bone metastases).
Confirmed diagnoses
Bone metastases were excluded in 101 cases (86%). Of the remaining 16 patients (14%), 12 prostate cancer patients and four breast cancer patients had metastases. Four patients died during follow-up (range, 130-705 days) after the initial planar bone scintigraphy.
In the patient-based analysis, PET/CT achieved the greatest accuracy (87%) in correctly identifying true-positive and true-negative cases, followed by SPECT/CT (85%) and planar bone scintigraphy (77%). PET/MRI reached an accuracy of 94% with a smaller sample size of 46 patients. All modalities missed the same two patients who were diagnosed with bone metastases 4.5 and 5 months after initial planar bone scintigraphy.
| Patient-based analysis for detecting bone metastases | ||||
| Planar bone scintigraphy | SPECT/CT | PET/CT | PET/MRI | |
| True positive | 9 | 9 | 12 | 6 |
| False positive | 3 | 7 | 2 | 2 |
| True negative | 82 | 90 | 94 | 37 |
| False negative | 5 | 6 | 3 | 1 |
The researchers also found a statistically significant difference between equivocal scans for planar bone scintigraphy (18), compared with SPECT/CT (5 scans, p = 0.004) and PET/CT (6 scans, p = 0.01). None of the 46 PET/MRI scans were deemed equivocal.
When the equivocal readings were categorized as malignant, planar bone scintigraphy misdiagnosed 24 (21%) patients, SPECT/CT incorrectly identified 17 (15%) patients, and PET/CT misdiagnosed 10 (9%) patients. SPECT/CT (14 patients, 12%) had the most misdiagnoses among benign equivocal readings, followed by planar bone scintigraphy (10 patients, 9%) and PET/CT (6 patients, 5%). PET/MRI misdiagnosed three (7%) patients in both cases.
When Löfgren and colleagues excluded equivocal readings, they found no statistically significant differences in sensitivity, specificity, PPV, NPV, or accuracy between the modalities.
| Diagnostic accuracy for detecting bone metastases | ||||
| Planar bone scintigraphy | SPECT/CT | PET/CT | PET/MRI | |
| Sensitivity | 64.3% | 60.0% | 80.0% | 85.7% |
| Specificity | 96.5% | 92.8% | 97.9% | 94.9% |
| PPV | 75.0% | 56.3% | 85.7% | 75.0% |
| NPV | 94.3% | 93.8% | 96.9% | 97.4% |
| Accuracy | 91.9% | 88.4% | 95.5% | 93.5% |
Interestingly, SPECT/CT (5 of 16, 31%), PET/CT (10 of 16, 64%), and PET/MRI (5 of 7, 71%) detected additional lesions in a relatively high percentage of patients with bone metastases. On a patient level, however, the three hybrid modalities correctly changed the tumor stage in a "relatively small fraction of patients compared to planar bone scintigraphy," the authors wrote.
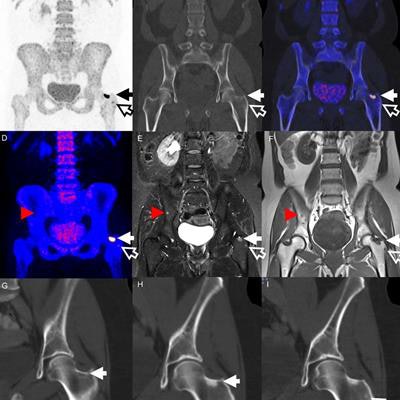
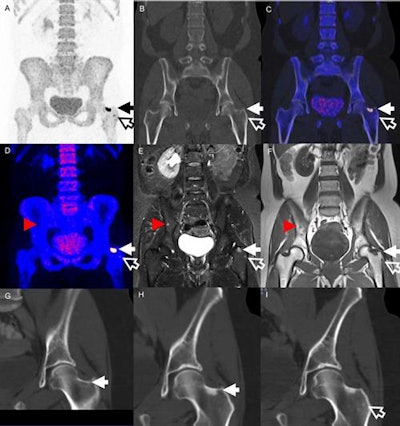 Images are from a 51-year-old woman treated for locally advanced breast cancer. Two lesions in the left hip were identified on both PET (A-C) and MRI (D-F) (solid and hollow arrows). The larger lesion could be found retrospectively on a diagnostic CT (G) one month prior to PET. CT two months after treatment (H) shows a sclerotic transformation of the lesion. The smaller lesion (I) has also turned sclerotic. MRI showed an additional lesion in the pelvic bone (red arrowheads) not identified on PET. Images courtesy of JNM.
Images are from a 51-year-old woman treated for locally advanced breast cancer. Two lesions in the left hip were identified on both PET (A-C) and MRI (D-F) (solid and hollow arrows). The larger lesion could be found retrospectively on a diagnostic CT (G) one month prior to PET. CT two months after treatment (H) shows a sclerotic transformation of the lesion. The smaller lesion (I) has also turned sclerotic. MRI showed an additional lesion in the pelvic bone (red arrowheads) not identified on PET. Images courtesy of JNM.The researchers noted that there were fewer equivocal readings with NaF-PET/CT and SPECT/CT, compared with planar bone scintigraphy. They attributed this result to the structural information provided by CT.
"There may well be significant differences in the sensitivity of SPECT/CT, PET/CT, [and] PET/MRI compared to planar bone scintigraphy, but a larger patient population or a patient population with a higher prevalence of bone metastases would have to be studied in order to demonstrate this," they wrote.