Awareness of possible artifacts and pitfalls in hybrid imaging is the first step in dealing with them, ECR 2019 delegates learned at today's session organized by the European Society for Hybrid, Molecular and Translational Imaging (ESHIMT). The presenters also discussed new types of problems and challenges that may occur with the clinical application of novel specific tracers.
Because of hybrid imaging's rapidly expanding application in routine scenarios, this session was aimed at general radiologists, not just specialists, according to Dr. Christina Pfannenberg, a PET/CT expert and the associate chair of the department of radiology at the Eberhard Karls University of Tübingen in Germany. While FDG-PET/CT has been widely adopted for staging and therapy response assessment in a variety of malignant tumors, greater demand for these studies means an increasing number of radiologists -- and oncologists -- without hybrid imaging training are now involved in interpretation of PET/CT scans on tumor boards or in routine reporting of other oncology imaging such as CT and MRI.
Presenting "Clinical pitfalls in FDG-PET/CT and PET/MR" this afternoon, Pfannenberg stressed that clinical interpretative pitfalls pose the greatest challenge to hybrid imaging. Therefore, it is crucial that doctors gain a basic knowledge of PET/CT and potential interpretation pitfalls to ensure accurate tumor evaluation and management, she told ECR Today ahead of the congress.
During her presentation, she plans to highlight the key imaging features of the physiological distribution of F-18 FDG and frequently encountered normal variants, a topic that sometimes can be problematic during interpretation.
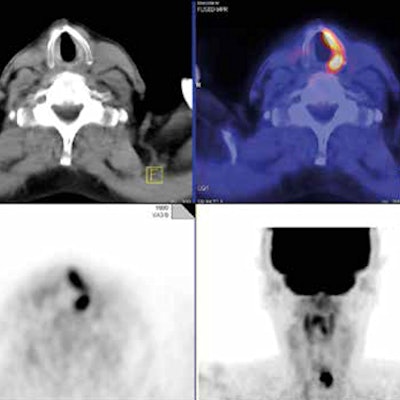
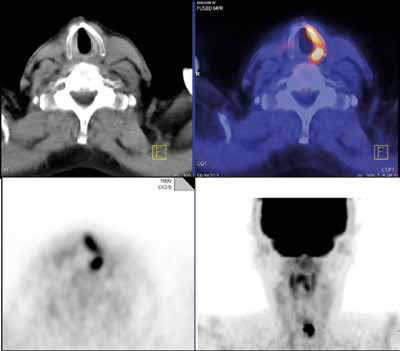 This clinical case shows a potential false-positive interpretation. A 70-year-old man with thyroid cancer and multiple past surgeries underwent restaging because of rising tumor marker. FDG-PET/CT showed asymmetric strong FDG uptake in the left vocal cord due to right recurrent laryngeal nerve palsy from prior surgery and tumor involvement. The compensatory activation of the nonparalyzed left vocal cord showing increased FDG uptake should not be misinterpreted as malignancy. Image courtesy of Dr. Christina Pfannenberg.
This clinical case shows a potential false-positive interpretation. A 70-year-old man with thyroid cancer and multiple past surgeries underwent restaging because of rising tumor marker. FDG-PET/CT showed asymmetric strong FDG uptake in the left vocal cord due to right recurrent laryngeal nerve palsy from prior surgery and tumor involvement. The compensatory activation of the nonparalyzed left vocal cord showing increased FDG uptake should not be misinterpreted as malignancy. Image courtesy of Dr. Christina Pfannenberg.There are several sites of normal physiologic uptake of FDG -- most intense in the cerebral cortex and less intense in the myocardium, liver, kidneys, and bone marrow. The uptake can be highly variable in the lymphatic tissue, salivary glands, thymus, muscles, ovary, testes, activated brown fat, and the gastrointestinal tract. One of the most important challenges is to correctly differentiate physiological uptake from these normal variants, and this differentiation can prove a great source of potential false-positive interpretation.
In addition to normal variants, other challenges stem from FDG not being a tumor-specific substance; increased FDG uptake may be seen in a variety of other benign conditions such as inflammation, treatment-related effects such as thymic hyperplasia after chemotherapy, sarcoid-like reaction after immunotherapy, and inflammatory response after radiotherapy. Benign tumors such as thyroid/colorectal adenoma also can lead to false-positive interpretation. Conversely, false-negative interpretations are possible in cases of low tracer uptake or high neighborhood activity, Pfannenberg continued.
"To avoid misinterpretation, FDG uptake should always be precisely correlated with the high-resolution contrast-enhanced CT, and all available clinical and other imaging data should be taken into account," she noted.
So how crucial is patient and protocol preparation to avoid misinterpretation, and are there any specific recommendations? Pfannenberg flagged the importance of standardization and urged everybody to check out the relevant guidelines from the European Association of Nuclear Medicine.
"The goal of preparation is to minimize tracer uptake in normal tissue while maintaining uptake in target tumor tissue," she said. "Preparation includes correct timing of PET/CT (more than 14 days after chemotherapy and three months after radiotherapy), fasting status in FDG-PET/CT, and interventions to reduce brown fat activity and hyperglycemia in diabetic patients. Oral CT contrast agents should be of low density with no barium, and patients should be instructed to stay relaxed and avoid talking and chewing after the injection of FDG."
The session also covered other aspects of hybrid imaging, namely the technical and methodological-related pitfalls and artifacts, addressed by ESHIMT President Prof. Thomas Beyer, PhD, deputy head of the Centre for Medical Physics and Biomedical Engineering at the Medical University of Vienna.
CT attenuation correction, performed in PET/CT to improve diagnosis, is prone to several errors due to methodological shortcomings associated with segmentation scaling methods and also CT transmission measurements, he explained. The most common errors include truncation artifacts and those arising from high-density implants and positive contrast agents. Specifically, high-density CT contrast agents, such as barium, can lead to an overestimation of FDG uptake. To prevent this, protocols must be optimized.
More frequently, errors from patient motion during the examination propagate through CT attenuation correction into the final images and lead to distortion bias of the reconstructed data -- and, potentially, mislocation. Again, protocols are the key to success here. In addition, artifacts and biases may occur from involuntary mistakes made during the setup and implementation of the imaging procedure, he added.
In a bid to provide useful pointers to attendees, Beyer outlined the principles of CT attenuation correction in PET/CT and discussed sources of artifacts arising from CT attenuation correction methodology and specific imaging workflow scenarios that are not optimized for routine PET/CT. He hopes that delegates will understand the methodological pitfalls of hybrid techniques and frequent potential image distortions and also grasp solutions to limit clinical misinterpretation arising from these artifacts.
Originally published in ECR Today on 27 February 2019.
Copyright © 2019 European Society of Radiology