Nearly a year passed between the announcement by the U.S. Centers for Medicare and Medicaid Services (CMS) that Medicare coverage would be available for low-dose CT (LDCT) lung cancer screening and issuance of the regulations that would allow claims to be submitted. The patient eligibility requirements and details for performing the exam were announced in February 2015, but it took the rest of the year before the billing and reimbursement particulars were known.
Finally, Medicare will pay for LDCT procedures performed on and after February 5, 2015, beginning in 2016. A 43-page decision memo from CMS defines in great detail the criteria that must be met by patients, physicians, and imaging centers for the scans to be eligible for reimbursement.
Below is a practical summary of the rules for performing and billing for these screening services.
Patient eligibility
Patients must be between 55 and 77 years of age; they must be asymptomatic, showing no signs or symptoms of lung cancer; they must have a smoking history of at least 30 pack-years; and they must be a current smoker or have quit smoking within the past 15 years. Cigar smokers or other noncigarette smokers are not eligible under Medicare's national coverage determination.
The initial CT screening must be ordered in writing by a qualified health professional following a visit that includes lung cancer screening counseling and shared decision-making. Subsequent screening exams must also be ordered in writing following any appropriate visit with a qualified health professional.
The written order must include the patient's date of birth, the number of pack-years in the patient's history, the patient's current smoking status (or years since quitting), a statement that the patient is asymptomatic, and the ordering practitioner's National Provider Identifier (NPI) number.
Facility eligibility
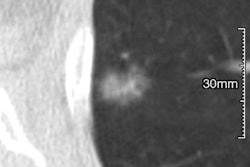
While there is no accreditation or certification required for imaging facilities, they must meet certain LDCT equipment requirements and use a standardized lung nodule identification, classification, and reporting system. The LDCT scanner must have a volumetric CT dose index (CTDIvol) of no more than 3.0 mGy for standard-size patients (5 ft 7 inches tall and approximately 155 lb) with appropriate reductions in CTDIvol for smaller patients and appropriate increases for larger patients.
The facility must also make smoking cessation interventions available for current smokers and submit specific data elements to a CMS-approved national registry. The American College of Radiology (ACR) formed the ACR Lung Cancer Screening Registry, which was approved for this program to enable radiologists to meet the quality reporting requirements and receive Medicare CT lung cancer screening payment.
This registry uses the ACR Lung Imaging Reporting and Data System (Lung-RADS), a quality assurance tool designed to standardize reporting and management recommendations for CT lung cancer screening, reduce confusion in lung cancer screening CT interpretations, and facilitate outcome monitoring.
Physician requirements
Radiologists must be board-certified or board-eligible with the American Board of Radiology or an equivalent organization, and they must have been involved in the supervision and interpretation of at least 300 chest CT exams in the past three years. They must also have met continuing education requirements in accordance with ACR standards. The services of physicians meeting these requirements will only be payable by Medicare if the radiology imaging facility meets the eligibility criteria described above.
Claim submission and payment
Services performed under this program on and after February 5, 2015, were eligible for payment beginning January 2016. Consistent with other preventive services such as mammography screening, Medicare has waived coinsurance and Part B deductibles for these lung cancer screening services. There should be no out-of-pocket expense, so imaging center staff should be notified not to collect such payments from these patients.
| Codes and payment levels* for LDCT screening | |||
| Description | Code | Professional component | Global payment |
| Counseling visit to discuss need for screening with LDCT | G0296 | 28.64 | $28.64 |
| LDCT scan for lung cancer screening | G0297 | $51.56 | $254.93 |
The shared decision-making visit may be billed on the same day as another evaluation and management (E&M) or annual wellness visit as long as the requirements for the counseling and shared decision-making visit are met. In such cases, a modifier -25 would be added to the G0296 code. As with a standalone LDCT counseling visit, no coinsurance or deductible would be associated with this billing.
The shared decision-making visit may be performed by a physician or other qualified nonphysician practitioner, such as a physician assistant, nurse practitioner, or clinical nurse specialist, if the services are ordered by any treating physician, including a primary care provider, within the context of a primary care setting.
Claims for these services must be accompanied by an appropriate ICD-10 code such as one of the following:
- Z87.891, personal history of tobacco use/personal history of nicotine dependence (not to be used for a current smoker)
- F17.2, nicotine dependence (for a current smoker)
Documentation
The imaging report should clearly indicate that the criteria necessary to qualify for reimbursement under this program were met. Some of this could be incorporated into templates with stock verbiage to indicate the following:
- "This exam was performed in a facility that meets the criteria for the LDCT screening program. Data regarding this exam was submitted to an approved registry."
- "The order for this exam indicates that it came as a result of a lung cancer screening counseling and shared decision-making visit that included all of the elements required of such a visit."
- "The radiologist interpreting this exam meets the CMS criteria for the LDCT lung cancer screening program."
The interpretation must include the elements required of the lung nodule identification, classification, and reporting system in use, along with the CT scanner make, model, and dose index information for each individual exam.
Conclusion
Radiologists interpreting LDCT lung screening exams under this new program should ascertain that the facilities in which they are practicing meet all of the eligibility criteria set out by CMS, or the radiologist's payment will be at risk. Imaging centers and hospitals will have an easier time submitting data to the registry and justifying reimbursement when necessary if a carefully designed intake form is used.
Such a form should include a checklist of all the eligibility elements for the patient and the requirements of the shared counseling visit. The radiologist's documentation must contain the minimum required data elements, and enough information about the overall patient evaluation to support reimbursement under Medicare's LDCT lung cancer screening protocol.
Carin Carlson is vice president of business development at Healthcare Administrative Partners (HAP), where she is responsible for all new business activity, including sales, marketing, product development, and strategic planning.
The comments and observations expressed herein are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.