We're making progress in the race to reduce radiation dose for CT lung cancer screening to ever-lower levels. But as dose drops, image noise grows. Fortunately, researchers are refining image processing techniques that can improve image quality while driving CT dose down to the level of a chest x-ray.
An international group has developed a microdose CT screening technique that reduced dose to as low as 0.13 mSv. The researchers then tested the ability of two image processing techniques -- computer-aided detection (CAD) and maximum intensity projections (MIPs) -- on phantoms to improve sensitivity, according to an article in the American Journal of Roentgenology (August 2016, Vol. 207:2, pp. 282-288).
What did they discover? Not all CAD algorithms are created equal, and radiologists reading MIP reconstructions of microdose CT images perform about as well as the best CAD working alone. What's more, the performance of both CAD and MIPs on low-dose images can vary widely based on myriad factors, including the algorithm, nodule size and type, and dose.
Optimizing low-dose screening
While current guidelines for low-dose CT lung screening call for radiation dose to be lower than 3.0 mGy, there is evidence that much greater dose reductions are possible, noted Dr. Lukas Ebner and colleagues from Duke University Medical Center; University Hospital Inselspital in Bern, Switzerland; and University Hospital Pitié-Salpêtrière in Paris.
 Dr. Lukas Ebner of Duke University.
Dr. Lukas Ebner of Duke University.For example, the mean effective dose for two-view chest radiography is about 0.1 mSv, but microdose chest CT can be performed at practically equivalent doses -- 0.06 to 0.16 mSv, the authors wrote. To be sure, the ultralow doses introduce image degradation in the form of higher noise compared to standard-dose CT, but the use of different processing techniques such as iterative reconstruction can mitigate the effects.
"As lung CT screening becomes more widely available, optimizing techniques for low-dose imaging protocols is critical to minimize radiation exposure in the screening population while preserving diagnostic accuracy for both solid and subsolid nodules," Ebner and colleagues wrote.
Two such techniques are MIP reconstruction and CAD. MIP reconstruction uses a simple postprocessing method that has been shown to boost nodule detection and temporal detection efficiency in both standard- and low-dose chest CT. As for CAD, studies have found that CAD software improves diagnostic sensitivity and specificity of nodule detection in lung cancer screening, according to the authors.
The type of reconstruction kernel can also have an impact. When using microdose CT, new data suggest that lower, softer reconstruction kernels may be superior to the sharper kernels commonly used in low-dose or diagnostic CT, they noted.
"Several studies have detailed the effects of radiation dose, reconstruction kernel, MIP, and CAD on lung CT image quality and nodule detection," Ebner and colleagues wrote. "However, to our knowledge, no comprehensive investigation has included all of these multivariate factors and examined their effect on diagnostic accuracy."
Testing it all
The study evaluated lung nodule detection on both standard-dose and microdose chest CT using two different CAD systems, one labeled CAD1 (syngo.CT CAD, VA 20, Siemens Healthineers) and the other labeled CAD2 (Lung CAD, IntelliSpace Portal DX Server, Philips Healthcare). They also analyzed the performance of radiologists reading MIP-processed images.
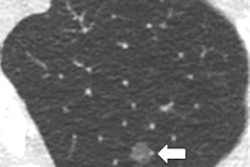
The chest phantom used in the study (N1, Kyoto Kagaku) is an anatomically accurate life-sized model of a male human torso, including a synthetic heart, trachea, mediastinum, and lung architecture, the authors explained. Standard-dose and microdose CT images were acquired on a 128-row CT scanner (Somatom Definition Flash, Siemens) and reconstructed using one of three kernels: i30, i50, and i70.
They scanned 133 ground-glass and 133 solid nodules with diameters of 5 mm, 8 mm, 10 mm, and 12 mm on 55 phantoms. Four readers blinded to other results evaluated the MIP images; one recorded the results of CAD1 and CAD2. Finally, sensitivities were calculated for CAD and MIP nodule detection on standard-dose and microdose CT for each kernel.
Microdose scans were acquired at 80 kVp and 6 mAs, with automated dose reduction disabled to minimize dose, and a high pitch factor of 2.2. Standard-dose scans were set at 100 kVp and 100 mAs. All other imaging parameters were the same.
For iterative reconstruction, level 3 iteration was applied to the raw datasets, and axial slices were reconstructed with the three different kernels (i30, i50, and i70) at 1-mm slice thickness for interpretation; there were no multiplanar reconstructions.
The results showed that radiation dose for microdose CT was significantly less than that of standard-dose CT (overall, 0.1323 mSv versus 1.65 mSv; p < 0.0001).
All techniques tended to perform best with the i30 reconstruction kernel. At that level, the CAD1 software operating on its own had comparable sensitivity to the radiologists reading MIP images. The CAD2 software trailed both techniques, however, in particular for sensitivity of ground-glass nodules.
| Performance of 3 image processing techniques at microdose radiation levels | |||||
| Sensitivity for solid nodules | Sensitivity for ground-glass nodules | Cumulative sensitivity | False positives per phantom | ||
| MIPs | 98.7% | 96.6% | 97.6% | 0.07 | |
| CAD1 | 99.1% | 92.9% | 96.0% | 8.3 | |
| CAD2 | 98.2% | 39.8% | 69.0% | 64.7 | |
"We think one of the main accomplishments of this research project is that we were able to show that ultralow-dose CT scans require soft kernels for best CAD system performance," Ebner wrote in an email to AuntMinnie.com. "Depending on the underlying software algorithm, our data show that lesion composition (solid versus ground glass) has a major impact on detection rates. Not completely surprising, soft-tissue kernels provide better results with low-dose CT, mostly because of reduced image noise. Another important finding, in our opinion, is the fact that MIPs are apparently still a valuable tool for lung lesion search when compared to CAD."
Did reader performance drop after the first detected nodule? A separate analysis found a substantial satisfaction-of-search effect after readers identified the first nodule in phantoms containing two lesions, the authors wrote. But the effect was null in phantoms with more than two lesions.
Importantly, there are major workflow differences between CAD and MIPs, Ebner told AuntMinnie.com. MIP images are created in the PACS system, so dedicated software isn't normally needed, and reconstruction takes just seconds.
On the other hand, "CAD analysis is usually more time-consuming," he said. After the source images are uploaded to the software, the results are ready in about 30 seconds for review by the radiologist.
"MIP reconstructions remain a valuable adjunct to the interpretation of chest CT for increasing sensitivity and have the advantage of significantly lower false-positive rates," the study team wrote.