The usefulness of neck CT angiography (CTA) in trauma cases is restricted by its cost, radiation dose, and contrast side effects, so careful clinical evaluation of potential candidates based on the internationally accepted criteria is essential, according to new research.
When used optimally, neck CTA is valuable for diagnosing a cerebrovascular injury (CVI), and routine screening of asymptomatic patients using neck CTA slightly increases the detection rate, noted Mohammed Alberawi and Hassan Aboughalia from the Radiology Residency Program, and Dr. Shatha Al Hilli, senior consultant in the clinical imaging department and head of the trauma and emergency radiology section, all of whom are based at Hamad General Hospital in Doha, Qatar.
CVI is a relatively uncommon event, having a reported incidence of around 1.6% in all trauma patients, but it has devastating complications, with a morbidity rate of 60% to 80% and mortality rate of up to 40%, they explained. Most CVIs are diagnosed after the development of symptoms secondary to brain ischemia. Screening of asymptomatic patients increased the incidence of CVI from 0.1% in hospitalized trauma patient to 1% and to 2.7% if the trauma score was more than 16.
"In the era of the advances and availability of various clinical imaging modalities, many proposed guidelines have been published, yet there is still no international agreed protocol," the authors wrote in an e-poster at the 2016 congress of the European Society of Musculoskeletal Radiology (ESSR). "Proper diagnostic evaluation and management protocol is required to decrease the morbidity and mortality rate, in addition to avoid nonindicated interventions."
Added value of neck CTA
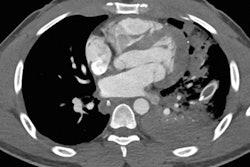
They conducted a study to determine the added value of routine neck CTA in all patients who were referred to Hamad General Hospital with a history of blunt/penetrating trauma or multiple traumatic events. The combined prospective and retrospective nonrandomized cohort study included all patients who underwent neck CTA on an emergency basis during 2015. Using the hospital's RIS/PACS, the group collected data on patients' demographics, mechanism of injury, and imaging findings, particularly neck CTA, CT scans of the brain and cervical spine, and any additional investigations like MR angiography or conventional angiography.
Standardized image acquisition protocols were used for all patients, and neck CTA was performed using the bolus-tracking technique on 64- and 128-slice scanners from Siemens Healthineers. Postprocessing maximum intensity projection/volume-rendered reconstructions were obtained, and then the images were interpreted by a senior neuro and emergency radiologist. Data collection and reviews were done by senior radiology residents. Most patients had previous nonenhanced brain and cervical spine CT scans before proceeding with CTA to assess for hemorrhage or fractures.
The sample size was 83 patients, and the majority of patients (94%) were men and the average age was 34. Most patients had suffered from multitraumatic events due to a road traffic accident (67%) or falling from a height (28%). Other less common mechanisms of injury were assault (3%) and penetrating neck injury (2%).
The CTA was normal in 91% of patients, with no evidence of trauma-related head and neck vascular injury. Only seven cases (8%) had an abnormal study, the abnormality affecting the vertebral arteries in five cases and the internal carotid arteries in two cases. Only one patient had an incidental nontrauma-related cerebral arteriovenous malformation.
The authors identified an associated cervical spine fracture and intraparenchymal hemorrhage in six out of the seven abnormal CTAs, and an isolated vertebral artery injury was seen in only one patient with a history of blunt trauma. In about 62% of normal CTA studies, patients suffered from a cervical spine fracture and/or head injury (e.g., craniofacial fractures, parenchymal hemorrhage).
"It is well established that symptomatic patients presenting following trauma with expanding hematoma, bleeding, or focal neurological deficit after a history of trauma must be evaluated by CTA or conventional angiography," they stated. "However, our study targeted asymptomatic patients or patients with other life-threatening conditions who were at risk of a missed CVI."
Lessons from the literature
Based on their literature review, asymptomatic patients have a CVI incidence of 1% to 3% versus 38% to 100% in clearly symptomatic patients, but no agreed protocol exists to determine which patients should be evaluated using CTA. The Denver modified screening criteria were developed based on the factors associated with increased risk of CVI, including a Glasgow Coma Scale score of < 6, petrous fracture, diffuse axonal injury, Le Fort II or III fracture, and the presence of a cervical spine fracture. Patients with any of these risk factors had a risk of 41% for CVI, and this risk increased to 93% in the presence of all five factors.
Adherence to these criteria should increase the rate of detection of CVI in selected patients, according to Alberawi et al.
The main drawbacks of performing neck CTA as a routine examination for trauma patients are the extra cost, radiation dose, and the risk of contrast-induced nephropathy, especially in patients with volume loss or pre-existing renal disease, they concluded.
To view the authors' clinical cases presented at ESSR 2016, click here.