SAN DIEGO - What's the best first-line diagnostic technique for assessing penetrating chest trauma? Dr. Savvas Nicolaou made the case for CT as the imaging modality of choice in a Friday presentation at the 2018 International Society for Computed Tomography (ISCT) symposium.
CT is ideal for the initial assessment of hemodynamically stable patients (blood pressure > 90 mm Hg) who present with acute penetrating trauma in the emergency department, Nicolaou, director of emergency and trauma radiology at Vancouver General Hospital in Canada, told meeting attendees. The technique can reveal the mechanism of injury and key anatomical landmarks, allowing for rapid triage and diagnosis.
"If you're suspecting a penetrating injury near the heart, perform a dedicated cardiac CT examination with functional analysis," he said. "It will be very useful; it can be life-changing for these patients."
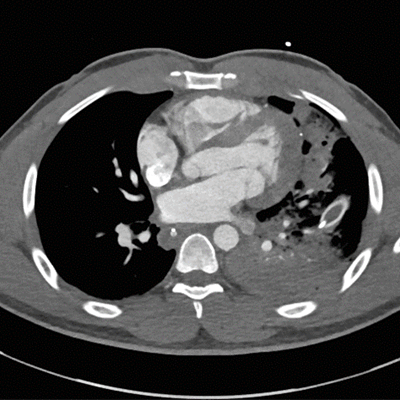
 Chest CT scan of a nail gun injury that caused fluid to leak out of the pericardial sac. All images courtesy of Dr. Savvas Nicolaou.
Chest CT scan of a nail gun injury that caused fluid to leak out of the pericardial sac. All images courtesy of Dr. Savvas Nicolaou.Shot to the chest
Though not as common as blunt trauma, penetrating trauma to the chest -- most frequently caused by a gunshot wound -- is associated with a considerably higher mortality rate, Nicolaou noted. Possible methods for the diagnostic evaluation of patients who do not require immediate surgery include chest x-ray, CT, echocardiography, and focused abdominal sonography in trauma (FAST).
X-ray was once the most widely used test for first-line diagnostic imaging, but advancements in CT technology have contributed to its rising use as the preferred modality in cases of penetrating trauma, he said. In particular, biphasic CT angiography (CTA) is well-suited to the task of highlighting potentially fatal injuries to the many arteries and veins in the chest.
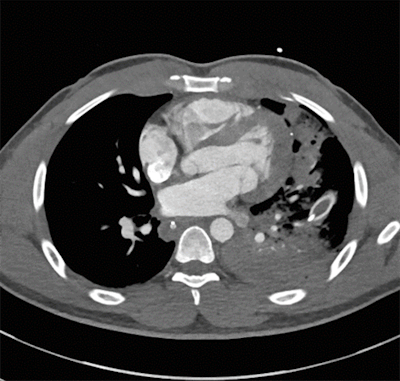 CT scan reveals a bullet fragment in the left ventricular wall (white speck in top right corner).
CT scan reveals a bullet fragment in the left ventricular wall (white speck in top right corner).There are three distinguishing signs on patients with penetrating trauma that prompt urgent evaluation with CTA as opposed to other imaging modalities:
- A central penetrating injury to the chest
- The presence of an artifact on the opposite side of its entry point into the chest
- Entry sites with corresponding exit sites
"If you can perform CTA earlier, it definitely provides more value for surgeons than doing chest x-ray," he told AuntMinnie.com. "[X-ray] can waste time and you need to act quickly to treat these critically injured patients."
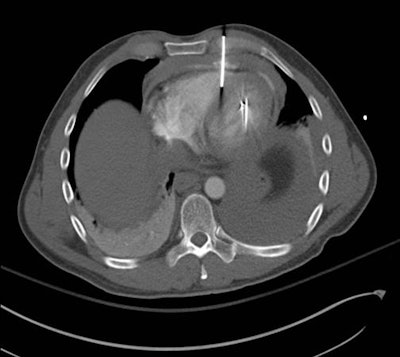
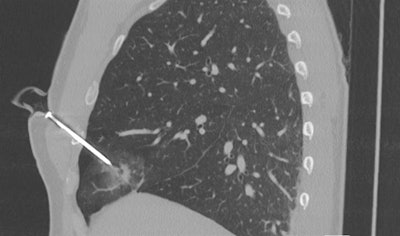 CT scan of a penetrating screw in the right side of the chest.
CT scan of a penetrating screw in the right side of the chest.CT has its advantages
In a prior case, Nicolaou and colleagues evaluated the x-ray image of a patient who had dozens of shotgun shell fragments lodged in the chest. Though x-ray confirmed the presence of the fragments, it neither revealed the extent of damage nor helped the physicians determine the best form of treatment. To clarify the situation, they performed a CTA exam, which indicated that there was no major injury to any vessels -- ultimately confirming that it was safe to discharge the patient without invasive surgery.
CTA can offer several other advantages for diagnosis in distinct regions of the body, especially concerning the site of injury:
- Heart: Penetrating trauma located within the "cardiac box," which covers the area between the nipples from the clavicle to the bottom of the rib cage, usually indicates significant cardiac injury. Clinicians should perform urgent, dedicated cardiac CT for such cases to confirm the need for surgical intervention, Nicolaou noted.
- Vasculature: Biphasic CTA is critical for visualizing vasculature since penetrating trauma is associated with a much higher risk of damage to the veins than blunt trauma is, he said.
- Esophagus: CT offers a higher specificity than x-ray does for detecting esophageal perforation, primarily by displaying indirect signs of injury. Delayed diagnosis and management of this type of injury could lead to respiratory failure and death.
- Lungs: CT is highly sensitive for pneumothorax as well as other pathology in patients with penetrating trauma that clinicians may easily miss on x-ray, such as pulmonary contusion and laceration.
- Diaphragm: Exploratory laparotomy is often required to confirm diaphragmatic rupture, but this imaging technique does not indicate the location of the injury relative to the rest of the anatomy. Both CTA and x-ray can help pinpoint the injury, though CTA has a higher detection rate than the roughly 50% detection rate of x-ray.
Making better radiologists
Further adding to the value of CT, the new advanced visualization technique of cinematic rendering can enhance the visualization of penetrating chest injuries. Nicolaou and colleagues have been using the "single-view" option to look at cinematically rendered CT scans for an initial impression. This feature allows users to click on and view just one of the photorealistic images quickly, rather than wait for the entire set of images to process.
"Cinematic rendering really shows the size and location of injuries; it more clearly shows how deep a wound is and what vital structures have been damaged," he said. "It gives the surgeons a better look of what they're dealing with and how complex the surgery might be ... generally changing the perspective of a surgeon for soft-tissue injuries and muscular injuries from penetrating trauma to the chest," he said.
For cases involving acute trauma, one of the chief aims of the radiologist is to bolster the other emergency and trauma physicians' understanding of the injury, Nicolaou noted. Yet this collaboration often ends up benefiting the radiologist, too.
"Collaborating with physicians from other specialties -- trauma surgeons and emergency physicians -- has made me a better radiologist," he said. "We go about the cases together in surgical acute rounds every week and we get the clinical feedback we need."