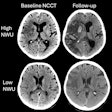
Clinicians in Northern Ireland reported that CT scans of a patient revealed a sizable black spot in the frontal lobe of the brain. This hypodense mark turned out to be a pocket of air that was compressing brain tissue as it seeped into the skull, according to a paper in BMJ Case Reports.
Referred to the emergency department by his general practitioner, the 84-year-old man had feelings of unsteadiness and recurrent falls for several months, as well as weakness in his left arm and leg for the past three days. Otherwise, the patient's physical exam, central nervous system exam, and blood test appeared normal, noted lead author Dr. Finlay Brown from Northern Ireland Medical and Dental Training Agency in Belfast and co-author Dr. Djamil Vahidassr from Antrim Area Hospital.
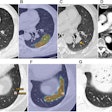
 CT scan displays an air cavity in the right frontal lobe as well as an osteoma in the paranasal sinus. All images courtesy of BMJ Case Reports.
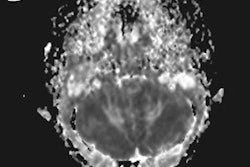
CT scan displays an air cavity in the right frontal lobe as well as an osteoma in the paranasal sinus. All images courtesy of BMJ Case Reports.Hoping to clarify the cause of the man's symptoms, the researchers turned to imaging. They acquired CT scans of the brain and found a 3.5-inch air-filled cavity, or pneumatocele, within the patient's right frontal lobe (BMJ Case Rep, February 27, 2018). Additional MR images of the head corroborated that the hypodense spot was, indeed, an air pocket and also uncovered an osteoma and signs of acute ischemia nearby.
Collectively, the findings suggested that the osteoma had gradually eroded the bone plate near the nasal cavity enough to allow air to enter the right frontal lobe in a "one-way valve effect."
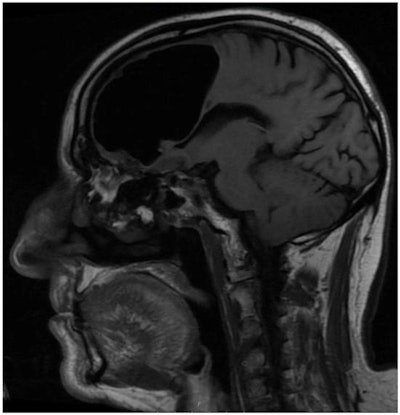 MR image shows the right frontal air-filled cavity.
MR image shows the right frontal air-filled cavity.After a period of observation and rehabilitation, the physicians offered the patient the option of a dual surgery that would clear out the pressurized air cavity as well as extract the bone tumor to reduce the risk of stroke. The patient decided not to undergo the procedure and elected to take a statin and anticlotting medication instead. In a follow-up meeting 12 weeks after the initial examination, the patient claimed that he no longer felt any left-sided weakness.
"When assessing patients presenting to primary or secondary care with new onset of neurological symptoms, one should have a low threshold for imaging to help distinguish between common and rare causes," the authors concluded.