Shared decision-making using a decision aid did not reduce the use of head CT for children with minor head injury, but it did improve parental knowledge and engagement and ultimately decrease downstream imaging, according to an article published online September 21 in JAMA Network Open.
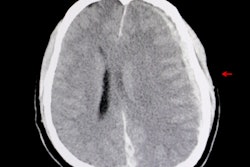
Researchers led by first author Dr. Erik Hess from the University of Alabama at Birmingham developed the Head CT Choice decision aid as a reference for emergency physicians and parents to review when deciding whether or not a pediatric patient should undergo a CT exam for mild head trauma.
They found that parents who participated in this shared decision-making process demonstrated increased knowledge of the risks of traumatic brain injury (TBI) and were more certain of their final decision, compared with parents who did not use the decision aid. Though the decision aid did not lead to a significant reduction in head CT use, it did reduce the patients' length of stay in the emergency room as well as the overall rate of follow-up imaging.
"These observations suggest that encounter-level decision aids can be viewed as bundled interventions that translate evidence into practice and improve decisional quality but may variably affect healthcare utilization depending on the degree to which current evidence guides practice," the authors wrote.
Parents need guidance too
Recent research has shown that U.S. clinicians continue to order a high rate of head CT exams for children presenting to the emergency room with minor head trauma, despite the implementation of the Pediatric Emergency Care Applied Research Network (PECARN) clinical prediction rules in 2009. One possible explanation for this could be that the prediction rules provide little guidance to parents on deciding whether their child should undergo CT or home observation.
To supplement the shared decision-making process, Hess and colleagues designed their Head CT Choice decision aid -- particularly for cases involving children who are at intermediate risk for clinically important TBI. They randomly assigned 172 clinicians from seven distinct healthcare institutions to use the researchers' decision tool or follow their usual management protocol for 971 cases. The average patient age was 6.7 years, 59% were male, and 26% were of nonwhite race.
Regardless of the form of decision-making employed (standard care or decision aid), the utilization rate of head CT for these cases was roughly the same. There were also no missed cases of clinically important TBI for either the standard care or intervention group.
However, the structured risk assessment and decision aid offered specifically to the intervention group led to statistically significant improvements in the parents' understanding of the risks involved as well as several measures of satisfaction.
| Standard care vs. decision aid for managing kids with head trauma | ||
| Standard care | Decision aid | |
| CT utilization rate | 24% | 22% |
| Length of stay in emergency room | 199 minutes | 176 minutes |
| Percentage of parents highly satisfied with decision | 44% | 52% |
| Parents' knowledge of risks | 5.3/10 | 6.2/10 |
"Parents who used a decision aid with their clinician had greater knowledge, less decisional conflict, greater physician trust, and greater involvement in CT decision-making," the authors wrote.
"A greater proportion of clinicians in the decision-aid arm would recommend the way they presented information to other healthcare professionals," they also noted.
Questions raised
Use of the decision aid was also associated with a statistically significant decrease in emergency department length of stay (p = 0.2), as well as significantly fewer blood tests and follow-up imaging procedures -- such as cervical spine and extremity x-ray -- within seven days after the patients were discharged.
"It is possible that parents who were engaged in imaging decisions using the decision aid were in closer communication with their care team, facilitating more timely discharge," they wrote. These parents may also have pursued follow-up exams less often, according to the researchers.
The similarity between head CT usage rates could be explained by the prior establishment of the PECARN guidelines at all of the participating sites, as well as the fact that the decision aid did not include details concerning the potential risks tied to CT radiation, noted Dr. Denise Dowd of Children's Mercy Hospital in Kansas City in an accompanying editorial.
"Use of the decision aid in sites not using the guidelines might demonstrate a different association with physician ordering of head CTs," she wrote.
Dowd also wrote that the study's findings raise a number of questions related to shared decision-making tools on the whole:
- How might discordance in racial background between a patient and physician affect outcomes?
- What about the parents' level of education and socioeconomic status?
- What type of training might clinicians need for using shared decision-making tools?
- How does using a decision aid affect the productivity of clinicians and their workflow?
"While many questions remain on the use of [shared decision-making] tools in pediatric acute care settings, tools which have the potential to support accurate and complete communication and engage parents in decision-making in busy emergency departments are more than welcome," she wrote.