For individuals with the novel coronavirus disease (COVID-19), several factors were associated with an increased risk of death in a new study, published online March 9 in the Lancet journal. Careful observation and blood testing could help clinicians identify these individuals at an early stage, researchers say.
In the observational study, Dr. Bin Cao of Capital Medical University and colleagues from China examined the data of 191 patients with confirmed COVID-19 at two different hospitals. The median age of the patients was 56 and nearly 30% died in the hospitals. They also had various comorbidities, the most common ones being hypertension (30% of patients), diabetes (19%), and coronary artery disease (8%).
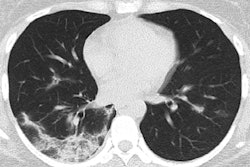
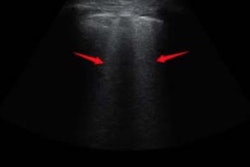
The researchers drew information from the patients' health records, laboratory test results, and chest CT and x-ray findings in order to determine the clinical course of COVID-19 over time.
After performing multivariable analysis on the data, Cao and colleagues identified three major risk factors associated with death from coronavirus in the patient cohort:
- Older age
- Symptoms of sepsis
- Having elevated levels of blood clotting factors
To be specific, the patients' risk of death increased by 1.1 times for each year of age, it increased by more than five times for those with a Sequential Organ Failure Assessment (SOFA) score high enough to indicate sepsis, and it increased by about 18 times for those who had a D-dimer blood test score exceeding 1 µg/mL.
| Risk factors associated with an increased risk of death from COVID-19 | |
| Odds ratio | |
| Age | 1.1 per year increase |
| SOFA score indicating sepsis | 5.65 |
| D-dimer blood test score > 1 µg/mL | 18.42 |
"Poorer outcomes in older people may be due, in part, to the age-related weakening of the immune system and increased inflammation that could promote viral replication and more prolonged responses to inflammation, causing lasting damage to the heart, brain, and other organs," said co-author Dr. Zhibo Liu from Jinyintan Hospital in a statement.
The researchers also found several findings from blood tests that were more prevalent among patients with severe COVID-19: a lower lymphocyte count, elevated levels of interleukin 6 (IL-6, a biomarker for inflammation and chronic disease), and elevated levels of high-sensitivity troponin I (an indicator for heart attack). In addition, they found that a much greater percentage of patients who died had respiratory failure, sepsis, and secondary infections, compared with those who survived.
Furthermore, the researchers tracked viral shedding in the patients and discovered that those who survived remained contagious for a median duration of 20 days, and as many as 37 days in one case. The duration of viral shedding appeared to be heavily influenced by disease severity, though the authors acknowledged that this finding was limited due to the low number of respiratory specimens collected and the minimal amount of genetic material detected in blood samples.
"The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. ... We recommend that negative tests for COVID-19 should be required before patients are discharged from hospital," Cao said.