Ten percent of patients with chronic obstructive pulmonary disease (COPD) who presented at the hospital with worsening respiratory symptoms and suspected pulmonary embolism (PE) proved to have the condition on CT pulmonary angiography (CTPA), according to a study published January 5 in JAMA.
French researchers found a 10% rate of PE in patients suspected to have the condition, in line with previous studies. More importantly, CTPA identified PE in 3.2% of COPD patients in whom it is not suspected. The findings suggest that CTPA could play a key role in screening for PE in this patient population, wrote a team led by Dr. Francis Couturaud, PhD, of the Hôpital de la Cavale Blanche in Brest, France.
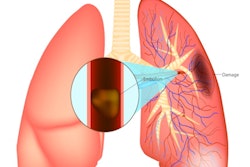
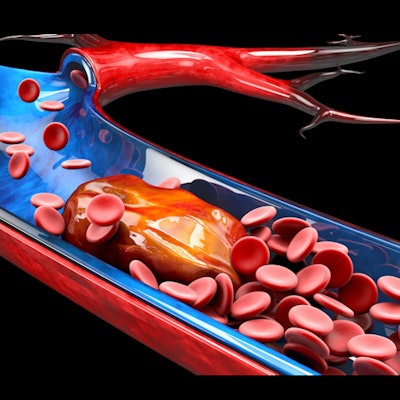
COPD is a common disease, with high morbidity and mortality, and it can be exacerbated by additional conditions like pulmonary embolism, the group noted. But how and when patients who present at the hospital with acute COPD symptoms such as shortness of breath should be screened for PE remains unclear -- since the signs of exacerbated COPD and those of PE can be similar.
Therefore, Couturaud and colleagues sought to address the question of how common PE is among patients with COPD who are admitted to the hospital with worsening respiratory symptoms.
The study included 740 patients with suspected PE admitted to one of seven French hospitals between January 2014 and May 2017. The final follow-up for the study occurred three months later.
On admission, patients were assessed for PE using the Geneva score; those with high probability of PE underwent CTPA and leg compression ultrasound within 48 hours of being admitted. Those with low probability of PE according to Geneva score had a D-dimer test. In those with negative D-dimer test results, clinicians excluded PE and patients were discharged without anticoagulant therapy.
Patients with confirmed venous thromboembolism on D-dimer testing received anticoagulants. All patients were instructed to return to the hospital immediately if any signs of venous thromboembolism or bleeding occurred between initial admission and a three-month follow-up.
The study's primary outcome was pulmonary embolism diagnosed within 48 hours of admission. The secondary outcome was discovery of pulmonary embolism at three-month follow-up in patients who did not have venous thromboembolism within 48 hours of hospital admission and did not receive treatments with anticoagulants.
Among the total patient cohort, 44 (5.9%) had confirmed pulmonary embolism and 1.4% had confirmed isolated deep vein thrombosis (DVT) on CTPA within 48 hours of admission.
| Prevalence of PE and DVT in patients presenting with exacerbated COPD symptoms | |||
| All patients | Patients with suspected PE | Patients without suspected PE | |
| Pulmonary embolism | 5.9% | 10% | 3.2% |
| Isolated DVT | 1.4% | 1.7% | 1.1% |
The Couturaud and colleagues found that the overall three-month mortality rate of 6.8% was higher among those who had venous thromboembolism at initial hospital admission (14 of 54 patients, or 25.9%) compared with those without (36 of 686, or 5.2%). The researchers also found that more of these same patients died during the follow-up period. Patients in whom PE was suspected had a higher prevalence of venous thromboembolism compared with those in whom it was not suspected (11.7% versus 4.3%).
The findings prompt the question of whether CTPA could be an effective way to screen for PE when COPD patients arrive at the hospital in respiratory distress, according to the group.
"Among patients with [COPD] admitted to the hospital with an acute worsening of respiratory symptoms, [PE] was detected in 5.9%," the group concluded. "Further research is needed to understand the possible role of systematic screening for [PE] in this population."