Adding CT pulmonary angiography (CTPA) doesn't necessarily improve the usual care protocol when it comes to identifying pulmonary embolism (PE) in patients with chronic obstructive pulmonary disease (COPD), according to a study published October 5 in JAMA.
Adding CTPA to the usual strategy of caring for patients hospitalized for worsening COPD didn't lead to any improvement in clinical outcomes, as measured by a basket of factors like death, hospital readmission, or thrombosis, according to a group led by Dr. David Jiménez, PhD, of Hospital Ramón y Cajal in Madrid, Spain.
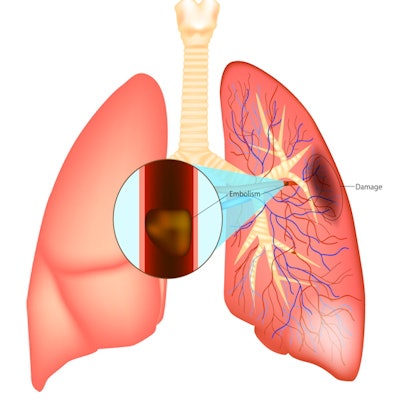
COPD is a dangerous disease, and pulmonary embolism is prevalent in patients experiencing aggravated COPD. Usual care for diagnosing PE includes D-dimer testing, supplemental oxygen, corticosteroids, antibiotics, and pharmacological thromboprophylaxis.
Many emergency departments have CT scanners available, and they have begun using CTPA with COPD patients as clinicians attempt to more actively search for PE in these patients, the group noted. But CTPA has downsides, and whether it is actually beneficial in this clinical scenario is unclear.
"CTPA is a time-consuming and burdensome investigation associated with radiation exposure, contrast reactions, and high cost," the authors wrote. "In addition, the need for an active detection strategy for PE needs to be balanced against the risk of exposing additional patients to anticoagulation, because the diagnosis may not always have clinical significance (i.e., subsegmental PE)."
Jiménez and colleagues evaluated the efficacy of CTPA for diagnosing PE through a study that included 737 patients who were treated for COPD between September 2014 and July 2020 in 18 hospitals across Spain. Study participants were randomized into two cohorts: One group of 370 that received usual care plus CTPA for diagnosing pulmonary embolism, and another group of 367 who received usual care alone.
The team measured primary outcome as whichever occurred first of the following three results:
- Nonfatal new or recurrent symptomatic venous thromboembolism (VTE)
- Hospital readmission for COPD
- Death from any cause within 90 days of being assigned to one of the two cohorts.
Secondary outcomes included nonfatal new or recurring VTE, deep vein thrombosis, or PE; readmission for COPD; and death from any cause within 90 days of being assigned to one of the two cohorts.
At 90-day assessment, 29.7% (110) of patients in the group that had usual care plus CTPA and 29.2% (107) of patients who just had usual care met the primary outcome criteria. The most common secondary outcome was readmission for COPD, but there was no significant difference between patients who underwent CTPA and those who did not.
| Comparison of outcomes by care protocol in patients with COPD | ||
| Outcome | Control group (usual care) | Intervention group (usual care plus CTPA) |
| Primary outcome (composite of nonfatal new or recurrent symptomatic venous thromboembolism, readmission for COPD, or death from any cause within 90 days) | 29.7% | 29.2% |
| Secondary outcome | ||
| Nonfatal new or recurrent symptomatic venous thromboembolism | 0.5% | 2.5% |
| Readmission for COPD | 25.4% | 22.9% |
| Death from any cause | 6.2% | 7.9% |
| Median time to discharge in days | 6 | 6 |
Adding CTPA to usual care for identifying PE in patients with chronic obstructive pulmonary disease doesn't seem necessary, according to the group.
"This multicenter randomized trial involving patients who required hospitalization for exacerbations of COPD showed that an active strategy for the diagnosis of PE (D-dimer testing and, if positive, CTPA) did not result in a lower percentage of patients having the composite outcome of nonfatal new or recurrent VTE, readmission for COPD, or death within 90 days after randomization," the authors concluded.




















