How accurate are two commonly used clinical models -- one from Mayo Clinic and another from Brock University -- for predicting whether incidental pulmonary nodules found on chest CT are malignant?
They could be better, according to a study published August 5 in the journal Chest. And the fact that these two models' accuracy is just "fair" -- and may lead to overestimations of cancer -- means that clinicians must take care when responding to incidental lung findings, wrote a team led by Dr. Anil Vachani of the University of Pennsylvania in Philadelphia.
"Overestimation of the probability of cancer has profound implications for clinical practice and suggests that clinicians may need to apply an intuitive 'correction factor' when making this determination, especially in never-smokers and at the higher end of predicted probability among ever-smokers," the group wrote.
Incidental findings are common
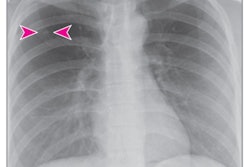
It's increasingly common for clinicians to find incidental pulmonary nodules in patients undergoing imaging for other indications, the group noted. And determining whether these nodules are malignant can be tricky.
"Although nodule identification is increasing over time, the frequency of lung cancer diagnosis after incidental nodule detection is not well defined," the authors wrote.
Surprisingly, there's a lack of population-based research regarding incidental nodule characteristics and the likelihood of cancer. Clinicians use prediction models to try to determine malignancy risk: Two common ones are the Mayo Clinic Solitary Pulmonary Nodule Malignancy Risk model for incidental nodules and the Brock University Calculator for nodules detected on lung cancer screening.
But how accurate are these models for discriminating between cancerous nodules and benign ones?
Vachani's group addressed this question via a study that included data from 23,780 Kaiser Permanente Southern California patients with incidental pulmonary nodules measuring larger than 8 mm identified on chest CT between 2006 and 2016.
The team tracked nodule characteristics by scanning dictated radiology report text and determined whether patients had received a lung cancer diagnosis within 27 months of the incidental nodule being identified (this time frame covers standard two-year follow-up as well as three months for diagnostic evaluation). The researchers then used the area under the receiver operating curve (AUC) measure to compare the cancer prediction accuracy of both the Mayo Clinic and the Brock models.
Of the total patient cohort, 9.9% had a lung cancer diagnosis within 27 months of discovery of the nodule. The study authors also found the following:
- 5.4% of people who had never smoked were diagnosed with lung cancer.
- 12.2% of former smokers and 17.7% of current smokers received a lung cancer diagnosis.
- 5.7% of people with 9 mm to 15 mm nodules were diagnosed with cancer, while 12.1% of those with nodules greater than 15 mm to 20 mm and 18.4% of those with nodules greater than 20 mm to 30 mm were diagnosed with cancer.
For the full study cohort, the Mayo model showed more accuracy than the Brock model, and it also had higher accuracy among the subgroup of patients who were current or former, Vachani and colleagues found. Both models overestimated cancer probability, however -- although the Brock model less so.
| Brock vs. Mayo models for predicting incidental lung nodule malignancy | ||
| Cohort type | Brock model AUC | Mayo clinic model AUC |
| Total patient cohort | 0.71 | 0.75 |
| Subset of current or former smokers | 0.72 | 0.73 |
"We found that pulmonary nodules measuring more than 8 mm in diameter are relatively common in clinical practice, and that approximately 10% of these nodules are lung cancers, with larger size and current smoking as important predictors of cancer," the team noted.
Experience and intuition
The Mayo Clinic model's slightly better accuracy over the Brock model may be due to how it was constructed, according to the authors.
"[The] Mayo model was developed in a sample of ever and never smokers with nodules detected incidentally on chest radiography, while the Brock model was developed in a population of current and former smokers with nodules identified on a screening low-dose CT scan," they wrote.
In any case, clinicians must make use of their experience and intuition when it comes to assessing incidental pulmonary nodules' cancer risk, corresponding author Dr. Michael Gould of Kaiser Permanente Bernard J. Tyson School of Medicine in Pasadena, CA, told AuntMinnie.com.
"We found that existing models had fair discrimination for cancerous nodules, but they overestimated the probability of cancer," he said. "Thus, clinicians should make an intuitive correction factor to decrease the probability when using the models to support clinical decision-making."