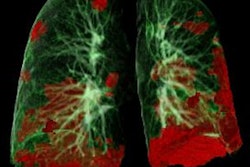
Scores of disease severity based on CT scans can help predict how COVID-19 patients will respond to noninvasive ventilation administered through an oxygen mask rather than through intubation, according to a study published September 11 in the Journal of Cardiothoracic and Vascular Anesthesia.
The study findings could improve outcomes in COVID-19 patients, wrote a group of researchers led by Dr. Luca Acari of Madre Giuseppina Vannini Hospital in Rome.
"[Our study found that] semiquantitative chest CT analysis at hospital admission provided highly reproducible prognostic information, especially in terms of responsiveness to [noninvasive ventilation]," the team wrote.
Noninvasive ventilation has proven to be an efficient tool for treating COVID-19, particularly when it is administered early after a patient is admitted, the group noted. But it performs poorly in some patients. To explore why, Acari and colleagues assessed whether there was a relationship between failure of noninvasive ventilation and a patient's rating on a numerical scale designed to rank the severity of a patient's COVID-19.
Described in a previous paper, the scale generates a score that's based on CT scans performed at four-day intervals. Readers score the disease involvement of each of the five lung lobes on a scale of 0 to 5, with 0 signifying no involvement and 5 signifying 75% involvement. The full scale ranges from 0 to 25.
In the current study, the researchers used the score to analyze scans of 112 patients admitted for COVID-19 pneumonia who received usual care -- including chest CT -- as well as respiratory support as needed.
Of the 112 patients, 59 (53%) received noninvasive respiratory support either with an oxygen mask without a ventilator or one connected to a ventilator. Of those who had this treatment, 38 had positive response and 21 had poor response; those with poor response were on average 78 years old, compared with those with positive response, who were 65 years of age on average.
The group found that those patients with poor response to noninvasive ventilation had higher chest CT scores than those with positive response, with an average score of 14 compared with an average score of 9 (p < 0.001).
Of the patients with poor response to noninvasive ventilation (mask plus ventilator), 42% went on to have respiratory support via intubation; of those who were treated with the mask alone, nine underwent intubated ventilation (8%). Twenty-eight of those who did not respond to noninvasive respiratory support either by mask alone or mask plus ventilator treatment died in the hospital, which the investigators attributed in part to their older age.
| CT scores in patients with positive and poor responses to noninvasive ventilation | ||
| Measure | Positive response | Poor response |
| CT score | 9 ± 3 | 14 ± 6 |
More research is needed to assess the relationship between chest CT scores and patient response to noninvasive ventilation techniques, according to the authors.
"Further studies are needed to fully assess whether routine implementation of CT score to guide clinical management might bring advantages in the care of patients with COVID-19 pneumonia," they concluded.