Adults who are on older blood-thinning medications have a significantly higher risk of a delayed intracranial hemorrhage (ICH) or death following brain trauma, according to research presented November 30 at the RSNA 2021 meeting in Chicago.
After conducting a retrospective study involving more than 1,000 patients with head trauma over three years, researchers led by Dr. Warren Chang of the Allegheny Health Network in Pennsylvania found that the group of patients who had been on older blood thinners such as clopidogrel (Plavix) and warfarin (Coumadin) had higher incidence of a delayed ICH occurring after the initial trauma and an initial negative CT exam.
Furthermore, taking aspirin along with any blood thinner may increase the risk of delayed brain hemorrhage.
"Given the high volume of our trauma patients taking aspirin and anticoagulants, this study will help to guide our care of closed head injury patients in emergency medicine and support efforts to use imaging resources appropriately," said co-author Dr. Thomas Campbell, system chair for emergency medicine of the Allegheny Health Network, in a statement from the RSNA.
The prevalence of patients taking blood thinners is increasing with the aging population. However, the incidence of delayed post-traumatic ICH in patients on different types of blood thinners with and without the addition of aspirin isn't well-established, according to Chang.
Although adults on blood thinners with head trauma typically receive a head CT, the standard of care beyond the initial imaging varies and different hospitals have different strategies for repeat imaging, according to the authors.
The researchers retrospectively reviewed the records of 1,046 patients in the Allegheny Health Network between January 1, 2017, and January 1, 2020, who had suffered head trauma and had an initial negative CT for ICH and went on to receive repeat imaging.
Of the 1,046 patients, 576 were taking one of the newer types of blood thinners, including apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa). The remaining 470 patients were on warfarin, clopidogrel, or another older medication.
Overall, 20 patients (1.91%) had a delayed hemorrhage and 3 patients (0.3%) died. All of the deaths were in the group of patients taking older blood thinners.
In other results, the researchers noted that 345 patients were receiving both blood thinners and aspirin. Of the 20 patients who had a delayed hemorrhage, 15 were taking an older type of blood thinner and nine of those were also taking aspirin. Furthermore, four of the other five patients who had a delayed hemorrhage were taking aspirin along with newer blood thinners.
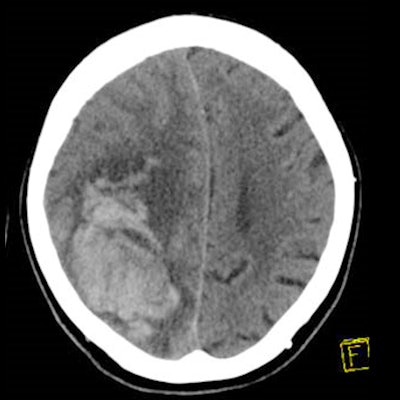
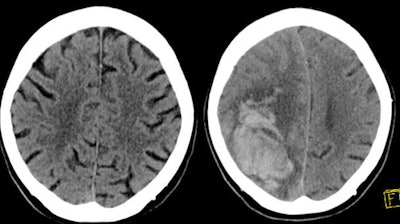 The left image shows the initial brain CT scan in a patient on both clopidogrel (Plavix) and aspirin who presented to the emergency department with head trauma with no intracranial hemorrhage. The right image shows a head CT obtained 24 hours later demonstrating a large parenchymal hemorrhage in the right frontal/parietal region. The patient died shortly after the second examination. Image and caption courtesy of Dr. Warren Chang and the RSNA.
The left image shows the initial brain CT scan in a patient on both clopidogrel (Plavix) and aspirin who presented to the emergency department with head trauma with no intracranial hemorrhage. The right image shows a head CT obtained 24 hours later demonstrating a large parenchymal hemorrhage in the right frontal/parietal region. The patient died shortly after the second examination. Image and caption courtesy of Dr. Warren Chang and the RSNA."Taking any blood thinner concurrently with aspirin significantly increased the risk of delayed hemorrhage, while taking one of the novel medications without aspirin significantly reduced the risk," Chang said.
Based on their results, the authors recommend that follow-up CT be performed on patients who did not have an initial ICH from head trauma but are on an older blood thinner or are taking any blood thinner along with aspirin. For those who are not on aspirin and are taking a newer blood thinner, follow-up CT is unnecessary unless there are external signs of trauma, according to the researchers.
"This study illustrates how innovative imaging can drive optimal patient care," said co-author Dr. Bethany Casagranda, chair of the Imaging Institute of the Allegheny Health Network. "In the end, I believe the recommendations of this work will save many lives."