Electronic cigarette (e-cigarette) or vaping-associated lung injury (EVALI) and COVID-19 can present similarly on imaging, but there are some findings that differentiate them, according to a February 11 International Society of Computed Tomography (ISCT) webinar.
In any case, there's no doubt that distinguishing between EVALI and COVID-19 can be a challenge, said presenter Dr. Seth Kligerman of the University of California, San Diego.
"They overlap, and most causes of acute lung injury these days are COVID, but EVALI hasn't gone away," he said.
Kligerman outlined both common and uncommon imaging findings for EVALI, citing research he conducted and published with colleagues in May 2021 in the journal Chest. He also described what imaging findings to look for to differentiate between EVALI and COVID-19.
In late 2019, the U.S. Centers for Disease Control and Prevention (CDC) declared an EVALI outbreak, then deemed it over in February 2020, according to Kligerman. But EVALI cases had been appearing before 2019 and have continued to appear, he said.
"[The EVALI outbreak] didn't start in 2019, and it didn't end in 2020," he said. "[At our institution] we continue to see one or two EVALI cases per month."
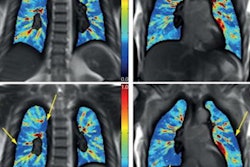
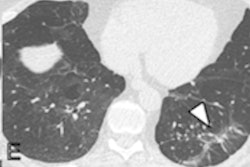
Like many acute lung injuries, the most common imaging finding for EVALI is ground-glass opacities with varying degrees of consolidation and tending to be predominant in the lower lobes of the lungs, Kligerman noted. He also listed these common findings -- data which came from the Chest study:
- Parenchymal lung sparing: 91%
- Lymphadenopathy: 63%
- Septal thickening: 51%
- Pleural effusions: 22%
- Centrilobular nodules: 7%
Parenchymal lung sparing can manifest in a few different patterns, with subpleural sparing most common (78%), followed by lobular sparing (59%), Kligerman said. He and his colleagues also found peribronchovascular sparing in 40% of EVALI patients. Almost a quarter (23%) of patients had all three sparing patterns.
In about 20% of EVALI cases, there is a mixed organizing pneumonia pattern, according to Kligerman.
"We see a mix between parenchymal and airway-centered organizing pneumonia patterns, with diffuse or lower lobe predominant ground-glass opacities and/or consolidation and upper lobe predominant, ill-defined centrilobular nodules," he said.
What are uncommon imaging findings for EVALI? Kligerman listed the following:
- Bronchial wall thickening: 11.9%
- Emphysema: 7.5%
- Bronchiolar dilation: 5.6%
- Fissural displacement: 3.7%
There may be uncommon parenchymal lobe organizing pneumonia patterns in EVALI patients as well: upper lobe (3.1%, and more common in older patients), consolidative (5.6%), and patchy (3.1%). Also rare, but possible, is an acute eosinophilic pneumonia (AEP)-like pattern and a pulmonary hemorrhage pattern, Kligerman told webinar attendees.
So how can clinicians differentiate EVALI from COVID-19? It's tricky because both will manifest signs of organizing pneumonia. But there are some key differences. Sometimes EVALI patients present with gastrointestinal symptoms such as nausea and vomiting, diarrhea, and abdominal pain, which don't tend to be symptoms of COVID-19 and may help distinguish the two conditions, he noted. Imaging findings uncommon with COVID-19 include the following:
- Centrilobular nodules
- Peribronchovascular sparing
- Lymphadenopathy
Identifying and treating COVID-19 has taken over much of the healthcare enterprise over the past number of years, but EVALI remains a concern, Kligerman concluded. And more research is needed to help clinicians identify it.
"Most EVALI cases are on the spectrum of organizing pneumonia to diffuse alveolar damage, and subpleural and perilymphatic sparing are common findings on imaging," he said. "But there are still a lot of unanswered questions regarding the mechanism of [EVALI] injury and the spectrum of its pathologic findings."