MRI shows promise as a noninvasive way to assess the short-term effects of vaping and tobacco smoking -- effects that manifest in different ways on medical images, according to a study published April 5 in Radiology.
The study findings may give clinicians a better understanding about how these two nicotine delivery systems affect users, providing them another tool in their lung assessment arsenal, wrote a group led by Dr. Sylvia Nyilas, PhD, of Bern University Hospital in Switzerland.
"[Our] results suggest that MRI indexes may be considered as a noninvasive test to complement pulmonary function testing [such as nitrogen multiple-breath washout or spirometry]," the team noted.
Vaping devices -- also known as electronic nicotine delivery systems or ENDS -- have been touted as a way to help people stop smoking tobacco. But it appears that people who vape to quit traditional cigarettes may continue beyond the quitting point, and this could translate into negative health effects.
"In laboratory analyses, ENDS is associated with a safer risk profile than conventional cigarettes," the group wrote. "However, vaping increases heart rate and blood pressure similarly to conventional tobacco smoking."
MRI is quite useful for identifying lung perfusion and ventilation impairment and assessing changes in the structure of lung parenchyma, Nyilas and colleagues explained. Previous research has suggested that functional MRI of the lungs could help identify early changes in ventilation and perfusion that aren't necessarily clear on traditional lung functional assessment tests.
In the current study, the investigators sought to explore the short-term effect of vaping and tobacco smoking on lung ventilation and perfusion using functional MRI.
They conducted a study that included 44 adults (10 were healthy control participants [never smokers], nine former tobacco smokers, 13 electronic nicotine device users, and 12 active tobacco smokers) who underwent lung function tests and noncontrast functional MRI scans before (MRI 1) and after (MRI 2) using vaping devices or smoking tobacco. Baseline assessment was performed after at least two hours of abstinence from vaping or smoking; the team measured lung perfusion and fractional ventilation impairment as percentages of affected lung volume.
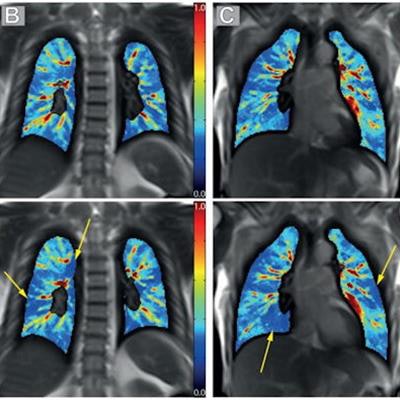
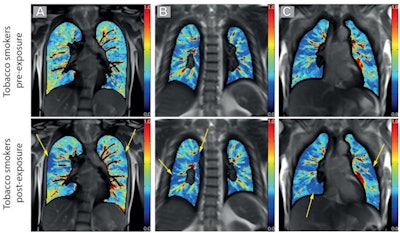 (A-C) Example of pulmonary perfusion images obtained by using noncontrast-enhanced matrix pencil MRI in three different tobacco smokers before exposure (preexposure) and after exposure (postexposure). The images before and after exposure were acquired at corresponding coronal section locations. Arrows indicate lung regions with decreased regional perfusion after the exposure to nicotine. Red corresponds to high values of ventilation amplitude and perfusion amplitude, whereas blue corresponds to low values. Images and caption courtesy of the RSNA.
(A-C) Example of pulmonary perfusion images obtained by using noncontrast-enhanced matrix pencil MRI in three different tobacco smokers before exposure (preexposure) and after exposure (postexposure). The images before and after exposure were acquired at corresponding coronal section locations. Arrows indicate lung regions with decreased regional perfusion after the exposure to nicotine. Red corresponds to high values of ventilation amplitude and perfusion amplitude, whereas blue corresponds to low values. Images and caption courtesy of the RSNA.Electronic cigarette (e-cigarette) users demonstrated a reduction in the percentage of lung impairment after exposure (which can impact ventilation) on the second MRI scan. In tobacco smokers, however, there was a decrease in lung perfusion after exposure (which impacts blood flow in the lungs), as indicated by a higher percentage of lung impairment. These were the only results that were statistically significant.
| Lung perfusion on MRI before and after vaping or tobacco exposure | |||
| Measure | MRI 1 | MRI 2 | p-value |
| E-cigarette users | |||
| Perfusion | 9.7% | 9% | 0.01 |
| Tobacco smokers | |||
| Perfusion | 8.6% | 9.1% | 0.03 |
More research is required to understand the effects of vaping and tobacco smoking, according to Dr. Seth Kligerman of the University of California, San Diego, who penned an editorial that accompanied the study.
"Although both cigarettes and vape pens can each serve as a nicotine delivery system, their mechanics and physiologic effects are unique, indicating the need for continued research," he wrote. "This also highlights that although we are only beginning to understand the short-term effects of vaping, the long-term effects are yet to be uncovered."