Combining CT lung imaging with machine learning may boost prediction accuracy for whether people with chronic obstructive pulmonary disease (COPD) will need further health services, according to a study published June 8 in Academic Radiology.
The ability to assess whether COPD patients will require additional healthcare interventions such as hospitalization could improve patient care, wrote a team led by Amir Moslemi of Toronto Metropolitan University in Canada.
"Patients with COPD are more likely to utilize healthcare services, have higher rates of hospitalizations and hospital readmissions, and higher rates of mortality," Moslemi and colleagues noted. "A better understanding of COPD patients at increased risk of healthcare utilization is therefore an important goal for improving COPD patient management."
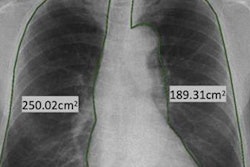
CT has been shown to be a useful tool for assessing the lungs of COPD patients through quantifying underlying factors that may be associated with poorer outcomes, while machine learning integrates demographic (age, sex, smoking status, pack years, and body mass index) and conventional lung function measurement data.
Moslemi's and colleagues tested the theory that adding quantitative CT imaging findings to a machine-learning model that included demographic and pulmonary function information would offer higher prediction accuracy of whether COPD patients would need further healthcare support compared to a model that only included the demographic and pulmonary function data.
The group collected lung function measurements and chest CT image data from 527 COPD patients who participated in the Canadian Cohort of Obstructive Lung Disease (CanCOLD) study between 2010 and 2017. These individuals underwent up to two follow-up visits (at one-and-a-half and three years postdiagnosis) and were asked to report any healthcare interventions, such as hospitalization or an emergency department visit for COPD or respiratory problems they had experienced in the 12 months previous to each. Of the total cohort, 35% (179) reported needing additional healthcare services in the 12 months before the follow-up visit.
The authors found that adding CT information to demographic and pulmonary function data improved the ability of clinicians to predict whether COPD patients would need further healthcare service support.
| Accuracy for predicting ensuing healthcare services use in COPD patients | |||
| Follow-up visit | Demographic/pulmonary function test measurements | Only CT measurements | All measurements |
| Visit 1 | 65% | 76% | 80% |
| Visit 2 | 66% | 74% | 78% |
| Visit 1 or 2 | 67% | 73% | 78% |
From both time and cost perspectives, "conventional" measurements to assess COPD are easier to gather than CT measurements from both time and cost perspectives, the team noted, but adding CT information to them increased prediction accuracy by up to 15%, depending on follow-up visit -- which could not only save healthcare costs but also improve patient care.
"Although this increase may seem small, identifying high-risk patients could lead to healthcare utilization prevention through earlier treatment initiation or more careful monitoring," the authors concluded. "It is clear that a small increase in prediction accuracy has the potential to prevent a large number of hospitalizations at the population level."