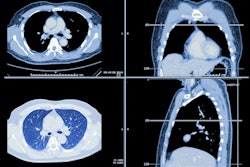
Incidental findings on low-dose CT (LDCT) lung cancer screening are relatively common. But are they being flagged -- and followed up -- appropriately? Perhaps not, if a recent study involving U.S. military veterans is any indication.
The American College of Radiology (ACR) has established a modifier for its LungRADS metric that indicates "clinically significant or potentially clinically significant" findings not related to lung cancer identified on LDCT. Yet use of it varies, according to a team led by Dr. Lauren Kearney of VA [Veterans Affairs] Boston Healthcare System. Kearney and colleagues assessed use of the college's "S" modifier in a population of U.S. veterans.
"[Our] study shows the prevalence of incidental findings in the VA population is considerable, especially when compared to lung cancer screening populations, [but] the labeling of incidental findings with an 'S' modifier and presence of recommended next steps is highly variable," the group wrote in a study published May 2 in Clinical Imaging.
In 2021, the U.S. Preventive Services Task Force (USPSTF) lowered the start age for annual lung cancer screening with LDCT from 55 to 50, expanding the pool of eligible individuals. With this expansion, lung cancer screening is identifying more incidental findings that should be followed, the group noted.
"How to manage incidental findings of lung cancer screening is one of the biggest challenges facing radiologists and primary care providers," they wrote. "Yet little is known about how the 'S' modifier is used in real-world practice, especially across centers nationally."
The team conducted a review of baseline lung cancer screening scans randomly selected from a national cohort of eligible U.S. veterans to assess application of the ACR's Lung-RADS S-modifier and how its use and follow-up recommendations vary across sites. The veterans underwent lung cancer screening at VA facilities between 2015 and 2019; of 37,908 veterans from 43 facilities, 2,183, or 5.8% had screening reports that included the "S" modifier.
The investigators found a more than 300-fold variation of "S" modifier use across the 43 sites (0.1% to 37.4%). They also found the following:
- 56% of patients without the "S" modifier in their imaging report had incidental findings; this is compared with the overall prevalence of use of the modifier of 5.8%.
- Of these individuals with the "S" modifier on their lung cancer screening report, 48.2% had a follow-up recommendation for the incidental finding, for which further imaging was the most common suggestion.
- There were 225 scans with incidental findings that did not include the modifier in the report; of these, only 11.6% included a follow-up recommendation.
The authors also found that radiologists commonly included a recommendation for incidental findings flagged with an "S" modifier (48% vs. 12%) but more than half of scans in the "S" modifier group lacked a recommendation and only 4.9% of the matched sample included recommendations for additional imaging or invasive procedures.
What's needed is further study on this phenomenon, especially as more people undergo lung cancer screening, according to Kearney and colleagues.
"Further investigation as to the underlying basis for this variation and of the clinical significance, benefit, and cost of evaluating incidental findings noted on lung cancer screening CT scans is necessary," they urged.