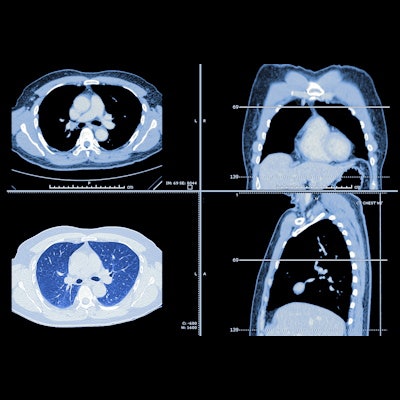
Most significant incidental findings discovered on low-dose CT (LDCT) lung cancer screening exams should be reported for further evaluation, suggest findings published May 8 in JAMA Internal Medicine.
Researchers led by Ilana Gareen, PhD, from Brown University in Rhode Island found that about one-third of participants in the National Lung Screening Trial (NLST) had significant incidental findings on their LDCT lung cancer screening study. Of these, nearly 90% were deemed reportable to referring clinicians.
"This large number of potentially clinically important significant incidental findings may be associated with a heavy burden of follow-up care and testing, with implications for patients, clinicians, and the healthcare system," the Gareen team wrote.
While previous research has demonstrated LDCT's efficacy in lung cancer screening, radiologists are challenged by addressing significant incidental findings -- potentially important abnormalities not tied to lung cancer -- and how best to report them to referring clinicians. Part of the conditions of the NLST included advising radiologists that such findings reported at baseline and stable at repeated screening did not need to be reported again.
Although some significant incidental findings may not pose an immediate threat and may not need invasive workup, others may be tied to the early diagnosis of life-altering conditions, the researchers noted. Gareen and colleagues wanted to describe these types of findings that were found in the LDCT arm of the National Lung Screening Trial.
Of 26,455 participants in this part of the trial, 10,833 (41.0%) were women, with the total population having an average age of 61.4. The trial also included 24,123 (91.2%) white individuals, 1,179 Black participants, and 470 Hispanic/Latino participants. The team reported that participants were set to undergo three screenings during the trial, with Gareen et al's study including 75,126 low-dose CT exams.
The researchers found that a significant incidental finding was reported for 8,954 participants (33.8%) who underwent low-dose CT. Of all screening tests that detected such a finding, 12,228 (89.1%) had one that was considered reportable to the referring clinician. This included a higher proportion of reportable findings among 7,632 participants (94.1%) with a positive screen result for lung cancer compared with the 4,596 (81.8%) who had a negative screen result.
The team also reported that emphysema accounted for the most significant incidental findings at 8,677 (43%). This was followed by coronary artery calcium at 2,432 (12.1%), and masses or suspicious lesions -- including kidney, liver, adrenal, and breast abnormalities -- at 1,493 (7.4%).
The researchers wrote that while classification was based on free-text comments, 2,205 of 13,299 comments (16.6%) could not be classified.
"The hierarchical reporting of final diagnosis in the National Lung Screening Trial may have been associated with an overestimate of severe emphysema in participants with a positive screen result for lung cancer," they added.
The study authors suggested that based on their findings, significant incidental findings should be reported to referring clinicians in a consistent manner. Established guidelines should be followed to minimize costs to patients, clinicians, and the healthcare system, they added.
However, they added that discovering these incidental findings could provide opportunities for early detection of non-lung cancer conditions in high-risk populations.
"Judicious classification and reporting of significant incidental findings may be used to assess the benefits or harms associated with their detection and guide improved management of participants with [findings] detected at lung screening," they wrote.
The team called for future screening trials to consider classifying significant incidental findings in the design phase. It also suggested that future work needs to evaluate such findings and their ties to patient morbidity and mortality, as well as focus on appropriate assessment approaches.





















