Opportunistic CT imaging bone density screening could increase osteoporosis screening by 113% without additional imaging -- and save the healthcare enterprise almost $100 million annually, researchers have reported.
The findings could improve patient care, especially for those who are at highest risk of fracture, wrote a team led by Soterios Gyftopoulos, MD, of New York University Langone Health. The work was a collaboration among researchers from the Harvey L. Neiman Health Policy Institute (HPI), NYU Langone, and Massachusetts General Hospital; it was published March 3 in the Journal of the American College of Radiology.
"Our study demonstrated the potential of CT to increase the rate of osteoporosis screening in the United States and the associated cost savings for eligible patients," it noted. "Male patients and patients with highest comorbidity burden would benefit the most from this expansion of screening."
Osteoporosis affects more than 50 million adults over the age of 50 in the U.S., and causes more than two million fractures per year, the group explained. The fractures have significant impact, not only on patients' quality of life but also on costs related to treatment; in fact, projected annual costs associated with hip fractures in the U.S. are estimated between $17 billion and $25.3 billion, with an increase of all-cause medical costs from approximately $22,000 to $70,000 per patient after fracture, the group wrote.
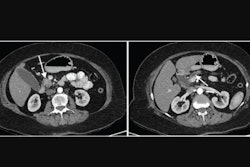
Bone density screening is typically conducted via dual-energy x-ray absorptiometry (DEXA), but its uptake among eligible individuals is low. That's where opportunistic CT imaging could come in, according to Gyftopoulos and colleagues.
To explore whether CT imaging could be an effective tool for this application, the investigators conducted a study that consisted of data from the Medicare 5% Research Identifiable Files from between 2015 and 2022; it identified all dual-energy x-ray absorptiometry (DEXA) procedures and contrast and/or noncontrast CT procedures using Current Procedural Terminology (CPT) codes -- tracking "outcomes of interest" such as osteoporosis screening imaging and fragility fractures of the hip or spine -- and calculating any annual costs related to osteoporosis that were avoided.
The study included 2.9 million beneficiaries, of whom 584,391 (20.2%) underwent DEXA and 658,703 (22.7%) who did not have a DEXA exam but did undergo at least one CT exam that included the L1 vertebral body (of these, 67.8% had CT imaging without contrast and 32.2% had CT imaging with contrast). The team reported that in both the noncontrast and contrast CT groups, there were 2,766 (0.6%) and 613 (0.3%) hip and 23,889 (5.3%) and 5,222 (2.5%) spine fragility fractures within a year of CT imaging.
Gyftopoulos' team found that using CT for osteoporosis screening could have a dramatic effect on both screening rates and healthcare costs:
- The osteoporosis screening rate would increase by 76% using only noncontrast CT studies and by 113% using all CT studies.
- If only noncontrast CT was used to identify osteoporosis and treatment was successfully implemented in 100% of eligible beneficiaries, this study population would see a medical cost avoidance in excess of $17 million.
- If any CT was used, potential annual treatment cost reduction for this study's population would be nearly $100 million and $2.5 billion for all 2023 Medicare fee-for-service beneficiaries.
The study underscores the "potential value of opportunistic CT imaging for patients with osteoporosis in terms of increasing the number of patients who could be screened and cost savings related to … early diagnosis and treatment," according to the authors.
"Underutilization of DEXA results in high rates of undiagnosed osteoporosis," co-author Casey Pelzl of HPI said in a statement released by the institute. "Our study shows that OCT has the potential to increase osteoporosis screening rates dramatically and subsequently help patients avoid fragility fractures, as well as the astronomical medical costs sustained after treatment."
Click here for the full article.