Becoming a living organ donor is no doubt a harrowing and emotional process. So should a potential lifesaver be subjected to a battery of imaging tests to determine his or her suitability? No, according to Korean clinicians who advocate a single modality exam with MRI for the preoperative evaluation of liver donors.
In related news, doctors from the Netherlands are uttering two little words that are generally not associated with MRI -- less expensive. They recommend using MR angiography (MRA) over digital subtraction angiography (DSA) for assessing living renal donors.
MRA for preop evaluation of kidneys
Earlier studies have demonstrated the clinical reliability of MRA in assessing living renal donors. The Dutch researchers decided to go one step further.
"We analyzed (MRA's) performance from a health policy perspective," explained Dr. Marc Kock and colleagues. "Given the previously reported high accuracy of contrast-enhanced MR angiography, we believe that it is important to measure the agreement with digital subtraction angiography, the impact on decision-making, and the hospital costs" (American Journal of Roentgenology, August 2005, Vol. 185:2, pp. 448-456).
Kock is from the departments of radiology and epidemiology and statistics at the Erasmus Medical Center in Rotterdam. His co-authors are from the departments of surgery and internal medicine.
For this study, the authors enrolled 42 potential donors with a mean age of 47. The subjects underwent imaging on a 1.5-tesla scanner (Signa CV/i, GE Healthcare, Chalfont St. Giles, U.K.). The MR protocol included T2-weighted single-shot fast spin-echo (FSE) and axial T2-weighted FSE with fat saturation. Two milliliters of gadopentetate dimeglumine (Magnevist, Schering AG, Berlin) were administered. Coronal 3D fast gradient-refocused echo (GRE) MRA was performed, as well as coronal 3D GRE MR venography and axial delayed gadolinium-enhanced 3D fast GRE imaging.
Finally, DSA images were obtained using a 38-cm field-of-view and an image matrix of 1,024 x 1,024 pixels (Integris V3000, Philips Medical Systems, Andover, MA; Angiostar Plus, Siemens Medical Solutions, Erlangen, Germany).
A vascular radiologist and a radiology resident evaluated all the images, and formed a consensus opinion. Findings from the MRA exams were discussed with the transplant surgeon to determine the impact of the test on decision-making. Costs were compared for the following: contrast MRA, DSA, and both exams together.
The results showed that contrast MRA depicted renal parenchyma or adrenal abnormality in 50% of the 42 cases. MRA proved to be excellent for detecting supernumerary arteries, although its performance was only moderate for arterial stenosis.
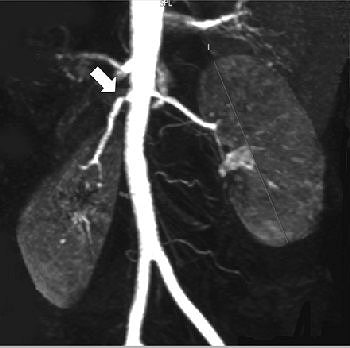 |
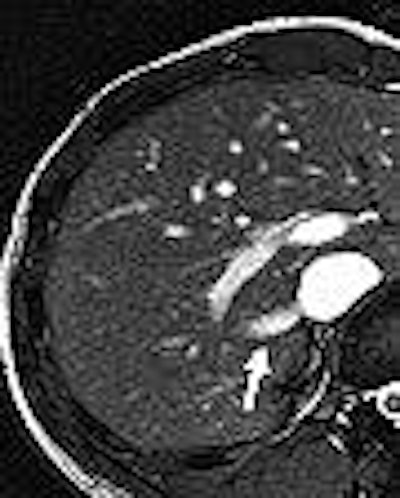
| Fifty-six-year-old healthy female living renal donor with stenosis of ostium of right renal artery. Above, volume maximum-intensity-projection MR angiography image using subtraction technique shows stenosis of ostium of right renal artery (arrow). Below, axial maximum-intensity-projection MR angiography image shows anterior origin of right renal artery with ostium stenosis (arrow). |
 |
"Based on only the contrast-enhanced MR angiography images, the decision as to which kidney to use for donation could be made in 40 (95%) of the 42 cases," the authors reported.
MRA results supported right-sided nephrectomy (the preferred side) in 52% of the cases and left-side nephrectomy in 43%. There were two cases in which MRA did not lead to a decision because of technical failures and patient movement during the scan.
In comparison, the decision on which kidney to use could be made in 88% of the cases based on DSA results. Among the 32 patients who underwent MRA and DSA, the latter only showed new findings in one case.
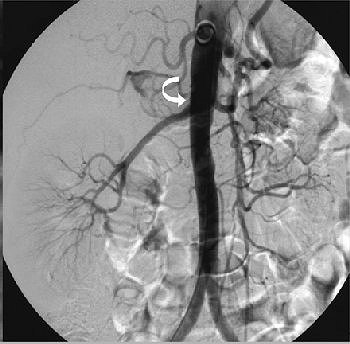 |
| Same patient as above. Digital subtraction angiography image that was insufficiently angulated does not show stenosis of ostium (arrow). Kock MCJM, Ijzermans JNM, Visser K, Hussain SM, Weimar W, Pattynama PMT, Krestin GP, Hunink MGM, "Contrast-Enhanced MR Angiography and Digital Subtraction Angiography in Living Renal Donors: Diagnostic Agreement, Impact on Decision Making, and Costs" (AJR 2005;185:448-456). |
In terms of cost, MRA alone was less expensive than DSA alone from a hospital perspective ($429 versus $539). The combination of MRA and DSA was the most expensive at $557. The authors pointed out that unlike a cost-effectiveness analysis, calculating "hospital costs inform us about the healthcare resources ... and can guide our choices in the setting of constrained resources."
Overall, the authors concluded that MRA had the edge in assessing living kidney donors, offering a superior ability to detect renal vascular abnormalities. In addition, MRA did not significantly alter kidney harvesting choices and was less expensive than DSA.
However, the group cautioned that MRA may fail to depict subtle renal artery stenosis so additional imaging may be necessary.
MRA for preop evaluation of liver
Examining the biliary tree of a potential liver donor can require as many as four different imaging tests: CT, conventional angiography, MR cholangiography (MRC), and MRA. With the latter, two different contrast agents are needed: mangafodipir trisodium for MRC and gadopentetate dimeglumine for MRA.
"The use of both contrast agents increases the cost of an examination and causes inconvenience to the patient.... A single dose of gadobenate dimeglumine potentially can provide a comprehensive evaluation of the hepatic parenchyma, vasculature, and bile ducts," explained Dr. Joon Seok Lim and colleagues from the departments of diagnostic radiology and surgery at Yonsei University College of Medicine in Seoul, as well as Yonsei's Brain Korea 21 Project for Medical Science (AJR, August 2005, Vol. 185:2, pp. 424-431).
Eleven candidates were enrolled in this study, and underwent MR on a 1.5-tesla unit (Gyroscan Intera, Philips Medical Systems). The sequences included breath-hold axial T1-weighted dual fast GRE, breath-hold axial T2-weighted turbo spine-echo with fat saturation, and breath-hold axial and coronal 2D balanced turbo field-echo.
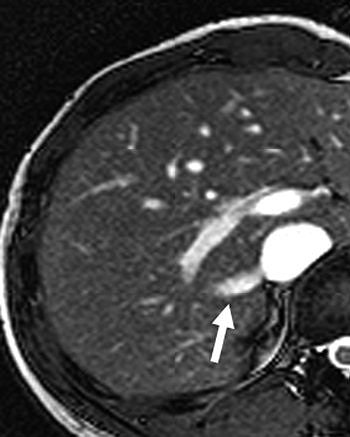 |
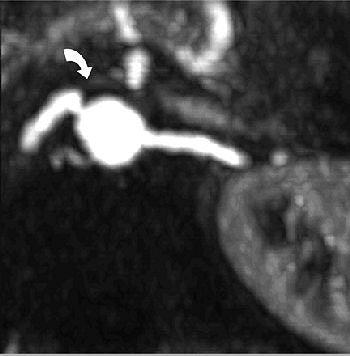
| Twenty-year-old man with large right inferior accessory hepatic vein. Balanced turbo field-echo images (above, axial image; below, coronal image) reveal a 7.3-mm right inferior accessory hepatic vein (arrow) entering inferior vena cava. Lim JS, Kim M, Kim JH, Kim SI, Choi J, Park M, Oh YT, Yoo HS, Lee JT, Kim KW, "Preoperative MRI of Potential Living-Donor-Related Liver Transplantation Using a Single Dose of Gadobenate Dimeglumine" (AJR 2005;185:424-431). |
 |
Dynamic MRA was performed in the coronal plane following a bolus of 0.1 mmol gadobenate dimeglumine (Multihance, Bracco Diagnostics, Princeton, NJ). Breath-hold T2-weighted MRC was performed with the same contrast agent. Finally, T1-weighted cholangiography was done. A radiologist and a surgeon prospectively evaluated the images in consensus. Two radiologists independently reviewed the various MRC images.
According to the results, prospective analysis indicated the vascular variants such as hepatic arterial variation and portal venous variation. On MR of the portal venous anatomy, a normal anatomy was identified in 10 of the 11 donors. Sixteen accessory hepatic veins were found in nine patients on MR of the hepatic venous anatomy. Biliary MRI identified biliary variants in two patients.
"The replaced common hepatic artery from the superior mesenteric artery in the donor candidate is known to be an important variant because extra steps are needed to remove the liver tissue," Lim's group stated.
The researchers found that the diagnostic confidence of T2-weighted MRC combined with the T1-weighted MRC with gadobenate dimeglumine was greater than that of T2-weighted MRC alone.
"Gadobenate dimeglumine can be used for dynamic imaging as an extracellular space agent in the early phase and the biliary contrast agent in the delayed phase," they stated. This information is important for the surgeon who will want to anticipate any additional components to the organ harvest surgery.
By Shalmali Pal
AuntMinnie.com staff writer
August 1, 2005
Related Reading
Retrograde cooling may protect kidney during radiofrequency ablation, July 14, 2005
Interventionalists see safer RFA with coregistered laparoscopic US, CT, June 27, 2005
CT tracks renal cancer recurrence after surgery, January 20, 2005
MR imaging accurately depicts prospective kidney donor anatomy, November 11, 2002
Copyright © 2005 AuntMinnie.com



















