Research has shown that women who smoke have a greater risk for developing osteoporosis. However, smokers who quit could actually see an increase in bone mineral density (BMD), according to Connecticut-based researchers.
On the other hand, any benefits derived from choosing a cigarette-free lifestyle may be for naught if primary care providers don't fully understand BMD test results and steer their patients in the right direction toward maintaining optimum bone health, said another team from the Cleveland Clinic Foundation.
First, Dr. Cheryl Oncken and colleagues looked at the impact of smoking cessation on BMD in postmenopausal women. "We hypothesized that women who quit smoking for one year would have a slower decline in BMD of the hip compared with those who continued smoking," wrote Oncken, who is from the Center on Aging at the University of Connecticut's School of Medicine in Farmington. Her co-authors are from the university's Storrs campus, as well as the VA Connecticut Healthcare System in Newington (Journal of Women's Health, December 2006, Vol. 15:10, pp. 1141-1150).
The study population consisted of 152 postmenopausal women who smoked at least 10 cigarettes a day. BMD of the hip, spine, wrist, and total body was measured by bone densitometry (Lunar DPX-IQ, GE Healthcare, Chalfont St. Giles, U.K.) at baseline and again one year after the women completed a smoking-cessation treatment program.
According to the results, smokers who had quit saw a 1.52% increase in hip BMD versus women who continued to smoke (0.43% increase). BMD improvement was seen in those who quit at the femoral trochanter -- 2.9% versus 0.6% for smokers. BMD changes at the femoral neck, radius, spine, and total body did not differ significantly between the two groups, Oncken's group stated.
Weight change was one of the main factors leading to increased BMD in women who gave up smoking, the researchers added, with the effects of cessation mediated by weight gain. Also, cessation was associated with an increase in bone alkaline phosphatase (BAP), which is a marker for bone remodeling, they stated.
The increase in hip BMD was particularly good news as decreased density in that area is a risk factor for fracture, the group concluded.
Secondary osteoporosis recognition
The word may be out that women of a certain age should undergo regular bone densitometry scans, yet healthcare providers are still not meeting the screening recommendations laid out by the National Osteoporosis Foundation (NOH) or the International Society for Clinical Densitometry (ISCD), according to Dr. Andrea Sikon and colleagues.
In this study, Sikon's group sought to determine the percentage of patients with DEXA scans who were referred for secondary testing by a primary care physician.
"Women with osteoporosis often are found to have secondary causes, most commonly including hypoestrogenemia, steroid use, excess thyroid hormone, and anticonvulsant use.... Low T-scores (≤ -2.5) do not necessary define primary osteoporosis, as this is only one possible diagnosis in a long differential of other potential causes of low BMD," wrote Sikon, who is from the Women's Health Center at the Cleveland Clinic Foundation in Ohio. Other contributors are from the departments of rheumatic and immunologic diseases and endocrinology (Journal of Women's Health, December 2006, Vol. 15:10, pp. 1174-1183).
All DEXA scans performed at the Women's Health Center from July 2002 to August 2003 were collected. These scans were assessed for abnormal results of low bone density/osteopenia (T-score of -1.1. to -2.4) or osteoporosis (T-score ≤ -2/5). In addition, the Z-score had to be -1.5 or less.
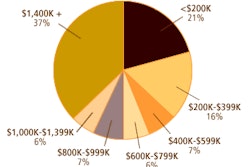
Referring physicians were categorized as a primary care provider (PCP) or specialist (internist, ob/gyn). A total of 31 providers (21 PCPs, 10 specialists) ordered DEXA scans in the study period. Possible secondary bone evaluations included conducting a complete blood count (CBC) and testing for thyroid-stimulating hormone (TSH) and blood urea nitrogen (BUN).
According to the results, of the 712 abnormal DEXA scans, 77 had low Z-scores and were recommended for secondary evaluation by the bone scan reader. However, only 49 of these 77 (63.6%) underwent additional evaluation at the behest of the referring physician. A woman was more likely to be sent on for additional tests by a specialist (95.1%) than by a primary care physician (27.8%), the study authors found.
The group suggested several possible reasons that PCPs, and specialists to some degree, were either missing or ignoring recommendations for workup, including a lack of understanding as to what constitutes appropriate secondary evaluation.
"At our facility, we have made efforts to unify report content and flow to simplify interpretation for the ordering physicians," the authors explained. "Outcomes of this change have not yet been assessed."
The group also found that referring physicians were often prescribing antiresorptive agents for osteoporosis without taking into consideration other mitigating factors, such as the patient's vitamin D levels.
By Shalmali Pal
AuntMinnie.com staff writer
January 31, 2007
Related Reading
Smoking-damaged arteries heal after quitting, December 13, 2006
MRS finds that smoke gets in the brain as well as the eyes, November 28, 2006
Antiacid supplement boosts bone mass, October 20, 2006
Cola consumption linked to weaker bones in women, October 11, 2006
Copyright © 2007 AuntMinnie.com