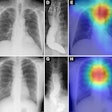
People with metabolic syndrome (MetS) and/or diabetes mellitus (DM) have greater progression of coronary artery calcium (CAC) than those without the conditions. In addition, the degree of progression in CAC predicts the risk of future cardiac events, according to a study in the Journal of the American College of Cardiology.
In more than 5,000 individuals participating in the Multiethnic Study of Atherosclerosis (MESA) who underwent baseline and follow-up coronary CT scans, an analysis of coronary artery calcium progression showed significant associations between coronary artery calcium progression and the presence of either MetS or DM.
Those with MetS (without DM) and those with DM (regardless of the presence of MetS) had a greater incidence of CAC compared with those who had neither condition. Those with both conditions had the highest association to CAC progression. As a result, CAC scores could be used to predict events in patients with either condition, wrote Nathan Wong, PhD, from the University of California, Irvine, and colleagues from several other U.S. centers.
"Subclinical atherosclerosis as evidenced by coronary artery calcium and carotid intima-media thickness is increased in MetS and DM, but no study has compared the incidence and progression of CAC across these conditions," Wong et al wrote. "Progression of CAC may be clinically important because persons experiencing [coronary heart disease] events have greater progression of CAC, and, recently, progression of CAC has been shown to predict all-cause mortality." (JACC, April 9, 2012).
The study compared CAC progression among individuals with MetS without DM, DM without MetS, and DM with and without MetS, in baseline and follow-up scans. All participants were free of cardiovascular disease at baseline. Exams were performed with EBCT scanners (n = 2852), MDCT scanners (n = 2,630), and multidetector EBCT scanners (n = 180).
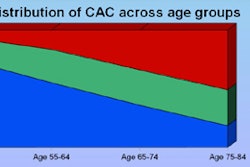
Overall the MESA study team scanned 5,662 participants (51% women, mean age 61.0 ± 10.3 years, ages 45 to 84) who received baseline and follow-up cardiac CT scans a mean of 2.4 years later in patients with MetS but no DM (25.2%), patients with neither MetS nor DM (3.5%), or patients with both conditions (9.0%). The authors compared the incidence and progression of coronary artery calcium in these patients compared to those with neither MetS nor DM (58%). Finally, Wong et al looked at CAC progression relative to coronary events over an additional 4.9 years after follow-up.
Data analysis included a chi-square test for categorical covariates, or an F test from analysis of variance for continuous covariants to assess bivariate associations between these groups, risk factors, and CAC score/volume measures. Relative risk regression was used to estimate the relative risk of incident CAC among subjects without calcium at baseline.
A total of 70 subjects who were excluded due to intervening coronary heart disease between baseline and follow up were more likely to have both MetS and DM (23%) and less likely to have neither (40%).
The highest clinical and risk factors among patients included systolic and diastolic blood pressure and triglycerides and waist circumference; waist circumference was highest and high-density lipoprotein was lowest in patients with MetS.
Growing risk
In subjects with no CAC at baseline, the risk of CAC progression grew with both DM and MetS.
"Compared with those with neither MetS nor DM, those with MetS (without DM) and DM (regardless of the presence of MetS) had a greater incidence of CAC," Wong et al wrote.
Overall results were similar to gender-stratified results, except that in women with DM but no MetS, findings were not significant. In results stratified by ethnicity, the relative risk for incidence of CAC was significantly greater for subjects with both MetS and DM among Chinese-Americans (relative risk 3.7), Hispanics (relative risk 2.2), and African-Americans (relative risk 1.8).
Relative risk regression for CAC incidence among 2,918 participants without baseline CAC by MetS and DM grouping
|
Among subjects with baseline CAC, progression also increased directly according to MetS and DM status. Subjects with both MetS and DM and those with DM but no MetS had the greatest progression in CAC; those with MetS but no DM had intermediate progression levels, Wong et al wrote.
Multivariate analysis of absolute progression of CAC Agatston score by 2,729 participants with baseline CAC
|
As for ethnicity, subjects in every group with both MetS and DM had the highest progression levels (mean-adjusted CAC volume differences of 15.3 -- 27.1 (p < 0.01) compared to those with neither condition, with the highest levels seen among Caucasians (23.4) and African Americans (27.1).
In an analysis by number of MetS risk factors, progression was greater only for subjects with three or more risk factors, Wong and colleagues wrote.
In the MESA cohort, "persons with MetS or DM have a greater incidence and progression of CAC than those subjects without MetS, and those with MetS (without DM) have an intermediate incidence and progression," Wong et al concluded. In previous studies, insulin resistance and DM have also been shown to relate to CAC progression, and CAC progression has been linked to total mortality.
Future events?
CAC progression was also examined relative to future coronary heart disease events. Total CHD events increased progressively according to the extent of change in calcium volume score in those with neither MetS nor DM, those with MetS but no DM, and those with both MetS and DM, Wong et al wrote.
"Progression predicted events in subjects with MetS without DM (adjusted hazard ratio: 4.1, 95% CI 2.0 -- 8.5, p < 0.001), and DM (adjusted hazard ratio 4.9 (95% CI 1.3 -- 18.4, p < 0.05) among those in the highest tertile of CAC increase from baseline versus no increase," they wrote.
The baseline calcium score is important to the understanding of the relationship of both DM and MetS to CAC progression, they wrote. From that viewpoint, baseline CAC could be considered a confounder, but "it can also be considered part of the causal pathway between risk factors such as MetS and DM and the progression of CAC," the group wrote.
"Such individuals likely had more rapid progression of CAC to begin with and continued to show greater future progression; hence, including baseline CAC in the model could condition out the effects that variables of interest [e.g., MetS and DM] may have to baseline." However, the results showed little differences in progression rates except for slightly faster progression in those with baseline CAC, Wong et al wrote.
As for limitations, the long 2.4-year interval between scans assumes a linear progression that may or may not be occurring, they wrote. Excluding 70 subjects for interval cardiovascular events prior to follow-up may well have influenced the results, since these individuals presumably have higher levels of both DM and MetS, leading to an underestimation of the link between the conditions and events. Even the debatable definition of MetS likely influenced the results.
"Persons with both MetS and DM have the greatest incidence and degree of progression of CAC," Wong and colleagues concluded.
Subjects with MetS but no DM have an intermediate degree of progression and incidence that falls between those of subjects with DM and those with neither condition. In subjects with MetS or DM, progression predicts the future risk of coronary heard disease events, they wrote.