Individuals found to have nonobstructive plaque at angiography are routinely sent home without being stented. But a new study from Colorado suggests that simply dismissing these patients and hoping for the best could be dangerous.
The study of more than 40,000 military veterans with nonobstructive coronary plaque found that their risk of heart attack is three to five times higher than that of patients without plaque. The findings could mean that a change in management is needed for patients with nonobstructive coronary artery disease (CAD).
Progressively greater risk
The risk of myocardial infarction (MI) or death over one year varied progressively with the extent of coronary artery disease, rather than changing abruptly depending on whether a plaque was flow-obstructing or not, according to the researchers. They presented findings from the U.S. Department of Veterans Affairs (VA) Clinical Assessment, Reporting, and Tracking (CART) study in June at the American Heart Association's Quality of Care and Outcomes Research 2014 Scientific Sessions.
"The results ... suggest that our standard black-and-white characterization that we've been making is a little too simplistic, and we need to change that to effectively counsel folks at risk and target them for preventive strategies -- either medicine or lifestyle changes," cardiologist Dr. Thomas M. Maddox, of the VA Eastern Colorado Health Care System, told AuntMinnie.com by telephone.
Maddox is an associate professor of medicine at the University of Colorado School of Medicine, and he is also the associate director for the VA CART program.
Flawed triage?
Patients with chest pain but no clinical or laboratory evidence of myocardial infarction are typically offered the option of elective angiography. During catheterization, their coronary plaques are often dichotomized into obstructive or nonobstructive stenosis to determine if they should undergo revascularization.
The problem with this decision-making process is that studies show no correlation between plaque stenosis and subsequent myocardial infarction. And the apparent disconnect between the need for revascularization and MI risk may discourage the pursuit of prevention strategies among these nonobstructive CAD patients.
Following angiography, "we would lump people with no evidence of coronary disease together with people who had nonobstructive disease, and say, 'You guys are all pretty low risk and we don't need to do anything else. Your chest pain is probably from something else. Go forth and prosper,' " Maddox said. "But the biology of coronary disease suggests that even folks with modest nonobstructive disease may not be as risk-free as we thought, so that's what we wanted to study: If you're normal, nonobstructive, or obstructive, what are your rates of heart attack down the road?"
Moreover, there are no longitudinal data on stable, nonobstructive CAD patients, Maddox said.
The researchers aimed to determine the prevalence and clinical characteristics of nonobstructive CAD in an elective catheterization population. They also wanted to compare one-year, risk-adjusted MI and all-cause mortality rates between normal, nonobstructive, and obstructive CAD patients.
Chest-pain patients nationwide
The group looked at all patients undergoing elective catheterization for chest pain, stable angina, ischemic heart disease, or a positive stress test between 2007 and 2012 at any of the 79 VA cath labs, excluding patients with known coronary artery disease.
They measured the extent of disease in two ways: the number of vessels affected, and the severity within each of those vessels, Maddox said.
Stenoses of 20% or less at angiography were considered negative, and nonobstructive disease was called for left main stenosis less than 50%, or 70% for all other coronary arteries. Obstructive disease included any left main stenosis greater than 50%, or any other stenosis greater than 70%.
The rates of heart attack and death within one year following angiography rose with increasing CAD severity, even among patients with nonobstructive CAD, Maddox said.
The rise in event rates was gradual and progressive, "rather than everybody with no obstructive disease having low rates and everybody with cardiovascular disease having high rates," he said.
| Adjusted 1-year MI rates by CAD extent | |
| Disease extent | Hazard ratio |
| 1-vessel nonobstructive disease | 2.87 (1.22, 6.77) |
| 2-vessel nonobstructive disease | 4.46 (1.99, 10.01) |
| 3-vessel nonobstructive disease | 4.93 (1.91, 12.76) |
| 1-vessel obstructive disease | 9.18 (4.31, 19.57) |
| 2-vessel obstructive disease | 17.29 (8.4, 35.57) |
| 3-vessel obstructive disease | 19.99 (10.31, 39.13) |
"If you have disease in one vessel, you're a little bit lower risk than two-vessel, and a little bit lower risk than three, but it's a very progressive relationship," he said. "It's a graded response, and it backs up the hypothesis that the more disease you have," the more MI and deaths will follow.
One-year death rates (and combined MI and death rates, not shown) also increased with CAD extent, he said.
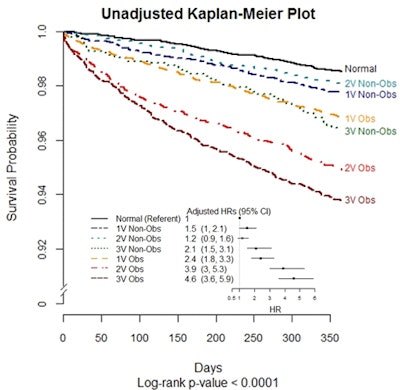 Image courtesy of Dr. Thomas Maddox and the American Heart Association.
Image courtesy of Dr. Thomas Maddox and the American Heart Association.Nonobstructive isn't nonsignificant
In summary, the researchers found that about 25% of patients in the elective VA catheterization population have nonobstructive coronary artery disease, and patients with nonobstructive CAD have 2.9 to 4.9 times the risk of MI relative to patients without plaque.
Key to the results is the fact that MI rates increased progressively with CAD extent, rather than abruptly between nonobstructive and obstructive CAD, Maddox said. The group found similar relationships between the death rate at one year and combined outcomes.
Maddox and colleagues will likely do a follow-up study looking at the effects of nonobstructive stenosis over longer follow-up periods than a year. With all 79 VA centers included, "we're enrolling the entire nation in this study," he added.
What should doctors be doing differently? Three main things, Maddox believes:
- Stop suggesting to patients that if they have nonobstructive disease, they are risk-free.
- Better appreciate the relationship between the increasing extent of disease and risk of heart attack, and adjust both counseling and preventive efforts accordingly.
- Set up studies to look at traditional preventive medicines, such as aspirin and statins, in nonobstructive patients to see if they provide meaningful risk reduction.
It so happened that nearly two-thirds of the patients were already taking such medications for indications other than known coronary disease, he said.
"My hypothesis would be that everyone with nonobstructive disease would benefit from an aspirin and a statin, but we would have to measure that risk-benefit to understand it a bit better," he said.
If it's true, then the approximately one-third of nonobstructive patients not on medication might have an indication to start taking it, he concluded.